Diet and Nutrition: Implications to Cardiometabolic Health
Melissa Johnson*
College of Agriculture, Environment and Nutrition Sciences, Tuskegee University, USA
Abstract
Cardiometabolic diseases and disorders continue to be the most significant and leading causes of morbidity and mortality in the United States, as well as globally. Among the cardiometabolic disorders, cardiovascular diseases (CVDs) have the greatest prevalence; other cardiometabolic disorders closely related to CVDs such as diabetes mellitus and Metabolic Syndrome (MetS) continue to contribute to the public health burden as well. Common risks for cardiometabolic disorders include biological (i.e. genetic predisposition, race, age, gender), demographic (socioeconomic status), dietary (dietary intake), behavioral (e.g., physical activity) and environmental (e.g., obesogenic, atherogenic, carcinogenic environments) characteristics. Paradoxically, dietary risk is both the most modifiable and least modifiable risk for certain diseases, as other modifiable and non-modifiable characteristics act in synergy to influence dietary intake. Although many inconclusive and conflicting research findings exist, the benefits of consuming a high quality diet are consistently valued and the role of diet in safeguarding cardiometabolic health cannot be underestimated. Diets rich in whole grains, non-starchy vegetables, and fruits, moderate in processed foods and refined grains, and consequently lower omega-6 to omega-3 fatty acid ratios appear to offer the greatest potential benefit. This mini review briefly summarizes the implications of diet and nutritional intake to cardiometabolic health.
Introduction
Often manifested as inflammatorily based diseases, cardiometabolic disorders may be one of the most irrefutable indicators of cardiometabolic health. Although no consensus definition of cardiometabolic health has been established, an individual’s cardiometabolic health (and cardiorespiratory fitness) may inversely be related to risk for overweight/obesity, insulin resistance, type 2 diabetes mellitus, hypertriglyceridemia, blood pressure, C - reactive protein concentrations, and cardiovascular disease (CVD)1-3. The 2011-2014 prevalence of CVD was approximately 36.6% of US adults (20 years and older), with non-Hispanic African American males (46.0%) and females (47.7%) exhibiting a significantly greater prevalence than other ethnic groups4. Further, the dynamic connection between CVD and Metabolic Syndrome (MetS) cannot be denied as epidemiological evidence has demonstrated overlapping risk, comorbidities and outcomes for both conditions5. Steady increases in the prevalence of MetS, defined as a cluster of clinical risk factors (i.e., abdominal adiposity, hypertension, dyslipidemia, insulin resistance) that significantly increase the risk for CVD, type 2 diabetes mellitus and certain cancers, have occurred over the years6,7. It is estimated that MetS is prevalent in ~1 in 4 adults, with rates increasing with increasing age8. The increasing pervasiveness of these near epidemic conditions may undesirably affect public health, as risks for comorbidities and premature mortality significantly increase with increasing prevalence. Therefore, mitigating the risks associated with cardiometabolic disorders and protecting cardiometabolic health is a paramount concern of public health professionals.
The Global Public Health Burden of Cardiometabolic Disease
Cardiometabolic disorders may not only adversely affect individual health but may compromise global public health as well. Unfortunately, racial and geographical variations in risk continue to exacerbate adverse cardiometabolic health outcomes9, particularly among vulnerable, at-risk underserved populations. Inconsistencies in measures and outcomes of cardiometabolic health further contribute to health disparities and challenges to global public health10. Appropriately, the prevention of cardiometabolic disorders requires an integrative approach that considers biological, dietary, behavioral, environmental, and other key characteristics. Because disease risk spans across the nature-nurture divide (Figure 1), a multidisciplinary prevention and treatment protocol must consider all of the factors involved. Among the key factors, diet is one of the most critical, as the diet provides both essential and non-essential nutrients required for cardiovascular health, cognitive functioning, immune function, homeostasis and the sustaining of life.
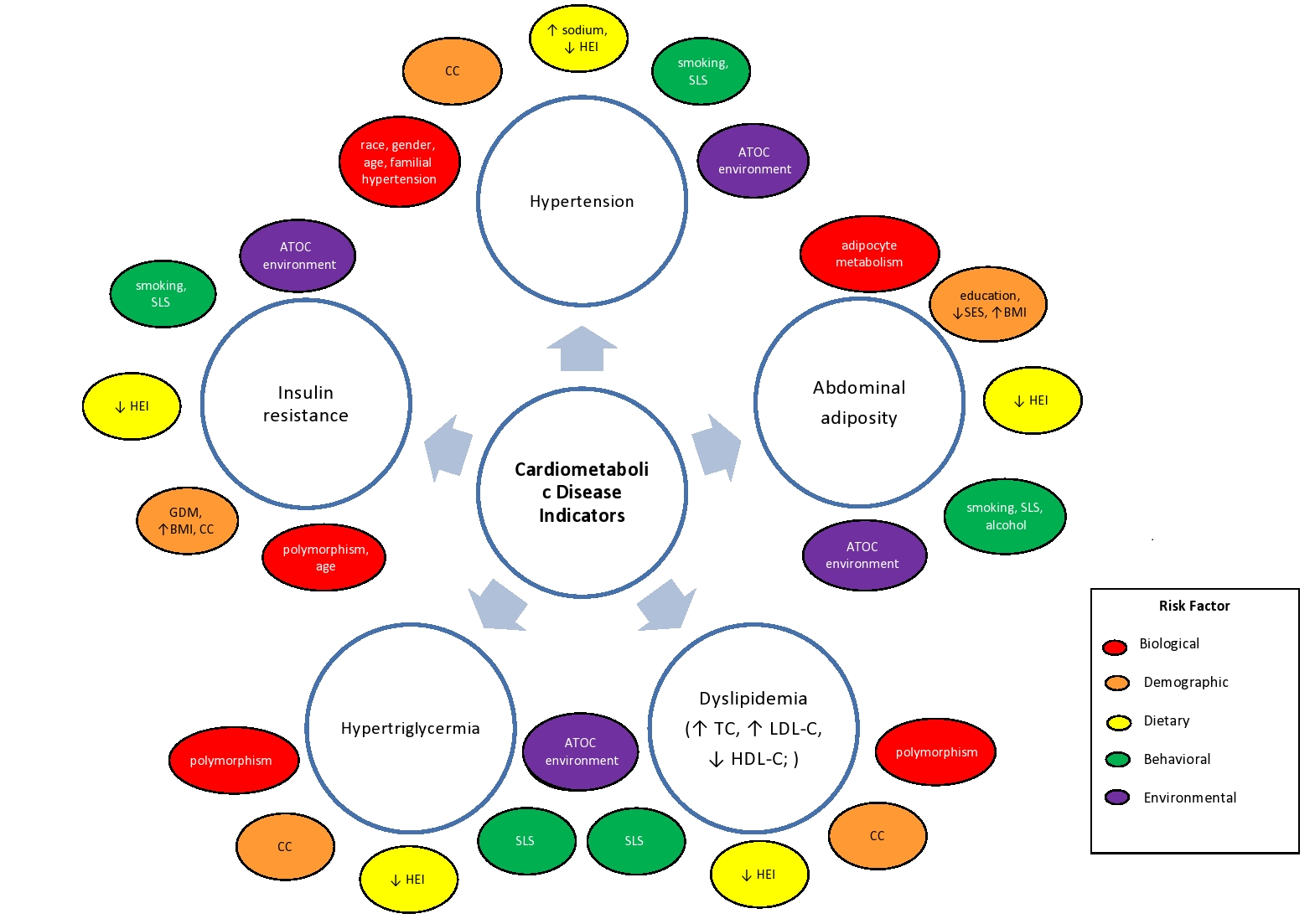
Figure 1. Simplified influence of biological, demographic, dietary, behavioral and environmental characteristics* on cardiometabolic disease indicators.
(*ATOC: atherogenic, toxicogenic, obesogenic, carcinogenic environment, an environment that facilitates the development of disease due to limited opportunity to engage in physical activity, acquire food (food desert), and receive preventive and/or treatment, health care resources and services, this environment may also be saturated with fast food restaurants/convenience stores (food swamp) and environmental toxins; BMI: Body Mass Index; CC: complication or comorbidity; GDM: gestational diabetes mellitus; HDL-C: high-density lipoprotein cholesterol; HEI: Health Eating Index, a measure of diet quality considering dietary variety and adherence to the Dietary Guidelines for Americans; LDL-C: low-density lipoprotein cholesterol; SES: socioeconomic status; SLS: sedentary lifestyle; TC: total cholesterol) **This figure is not exhaustive and does not capture the vast risks for cardiometabolic disease.
Dietary/Nutrition Transition
Although abundant in animal products, the earlier hunter-gatherer diet was not considered atherogenic in nature11. The complementary higher intakes of dietary fiber, antioxidants, phytochemicals, bioactive compounds, vitamins, mono- and polyunsaturated fatty acids -from plant sources and a lower omega-6/omega-3 fatty acid ratio could have in fact provided cardio-protection. Other lifestyle and environmental characteristics (e.g. greater physical activity, less exposure to environmental toxins, lack of cigarette smoking) are believed to have synergistically contributed to the cardiometabolic health of the hunter-gatherer as well. However, during the nutrition transition the “Westernization” of food production resulted in increased availability of processed foods, excessive intakes of calories, sugar, sodium and fat, and decreased diet quality12. This nutrition transition also resulted in a shifted increase in omega-6 fatty acids intake and an ensuing elevation in the dietary omega-6/omega-3 fatty acid ratio13,14. Consequently, the more Westernized dietary pattern (and lifestyle characteristics) have led to nutritional deficiencies/toxicities, physiological imbalances, chronic inflammation and disease15,16. Not surprisingly, these atherogenic, obesogenic, diabetogenic, carcinogenic, and toxicogenic diets have facilitated the pathogenesis of chronic, diet-related diseases such as CVD, diabetes, obesity and certain cancers17,18. Similar trends in chronic diet-related diseases such as malnutrition (over- and undernutrition), obesity, diabetes, dyslipidemia, hypertension and cardiovascular diseases are evident in both developed and developing countries19. Even more concerning is the observational evidence that trends in risk (e.g., dietary, socioeconomic, physical activity) emerge in childhood and continue into adulthood, predictive of cardiometabolic health20-22.
Dietary Protection of Cardiometabolic Health
In light of the cardiometabolic threats introduced during the nutrition transition, the year-round availability of foods once considered seasonal, provides an opportunity to improve diet quality. The Mediterranean Diet, characterized as being rich in plant-based foods and having a lower omega-6/omega-3 fatty acid ratio, has yielded positive nutritional genomic effects on cardiometabolic health23-25. Non-nutritive bioactive compounds commonly found in plants may favorably influence nutrigenomics and shift the balance in the direction of health promotion and disease prevention by selectively amending specific metabolic pathways and attenuating inflammatory mechanisms implicated in disease pathogenesis26,27. In addition, research has demonstrated the ability of green leafy vegetables and the dietary omega-6/omega-3 fatty acid ratio to modify disease risk by influencing fatty acid profiles, blood pressure and markers of inflammation in an animal studeis28,29. Although caloric restriction has been endorsed to benefit metabolic health30,31, it has been suggested that the macronutrient content of the diet, rather than total caloric intake, guides cardiometabolic health32. Interestingly, the influence of macronutrient intake on body fat, blood pressure and blood lipids, appears to vary among males and females33. In addition to the macronutrients, other dietary components may support cardiometabolic health by facilitating specific processes that optimize cardiometabolic functioning (Figure 2).

Figure 2. Potential cardiometabolic effects of dietary components§.
§ Non-nutritive components of food including, but not limited, to phytochemicals (carotenoids, flavonoids, isoflavones, polyphenols), isothiocyanate, phytosterols and tannins.
The Omega-6/Omega-3 Fatty Acid Ratio
The essential omega-3 and omega-6 polyunsaturated fatty acids have an array of physiological functions in cellular integrity and viability, immune function, inflammation and disease risk34,35. Although the ability of omega-3 fatty acids to prevent disease in epidemiology studies have yielded conflicting results36-38, it has been suggested that omega-3 fatty acids may exert beneficial actions in reducing the risks associated with MetS by influencing oxidative status, glucose homeostasis, lipid metabolism and adiposity39. It has been proposed that reducing omega-6 fatty acid intake (below the current recommended levels of 5% to 10% of total energy) may potentially increase risk for CVD40. Considering this, it has been suggested that individuals consume “optimal” intakes of omega-3 and omega-6 polyunsaturated fatty acids that will not only prevent essential fatty acid deficiency, but decrease chronic disease risk40. Racial genetic variations in omega-6 and omega-3 fatty acid metabolism have been observed41-44 and may offer a fractional explanation of the disparities in disease prevalence among certain racial groups.
The delicate balance in omega-3 and omega-6 fatty acids intake not only affects the production of eicosanoid metabolites that facilitate inflammatory and other homeostatic responses, but is central in the pathogenesis of diseases with an inflammatory epicenter, such as cardiovascular diseases, diabetes, degenerative diseases and mental disorders45,46. Imbalances in the ratio of omega-6 to omega-3 fatty acids may lead to imbalances in endogenous mediators and gene-nutrient interactions with biological consequences that may influence disease risk47-49. Adequate intakes of essential omega-3 and omega-6 polyunsaturated fatty acids, combined with dietary, behavioral and other lifestyle characteristics that promote health are believed to reduce – by default, risk for chronic disease as well50-52.
Conclusions
The drastic transition from dietary patterns abundant in plant-based foods (e.g., whole grains, legumes, vegetables, fruits) and lean meats to less plant foods and more refined grains and processed foods, rich in calories, added sugar, sodium, and (total and saturated) fat, have unfavorably affected human health. The gradual decline in diet quality, together with other demographic, behavioral and environmental characteristics have resulted in the emergence and sustaining of diet-related, chronic diseases. The initiation of specific metabolic pathways following nutrient intake expedite nutrigenomic and nutrigenetic outcomes that may beneficially or adversely affect cardiometabolic health. The typical Western dietary pattern exacerbates the risk for cardiometabolic disease, as it enhances a physiological microenvironment that encourages the initiation of pro-inflammatory pathways.
Because diet (and nutrition) directly affect the genome, transcriptome, proteome and metabolome, subsequent alterations in cardiometabolic health follow alterations in dietary intake. Dietary patterns aimed at reducing cardiometabolic risks should be balanced in plant-based foods, lean meats, essential omega-3 and omega-6 fatty acids and non-nutritive bioactive compounds. Optimizing nutritional intake and diet quality therefore becomes paramount to safeguarding cardiometabolic health. As cardiometabolic health is of public health concern, minimizing risk for adverse cardiometabolic health outcomes should begin during childhood, and quite possibly prior to conception.
Acknowledgement
This work was supported by the Tuskegee University College of Agriculture, Environment and Nutrition Sciences George Washington Carver Agricultural Experiment Station.
Conflict of Interest
The author declares that there is no conflict of interests.
References
- Lotta LA, Abbasi A, Sharp SJ, et al. Definitions of Metabolic Health and Risk of Future Type 2 Diabetes in BMI Categories: A Systematic Review and Network Meta-analysis. Diabetes Care. 2015; 38: 2177-2187.
- Blackburn P, Lemieux I, Alméras N, et al. The hypertriglyceridemic waist phenotype versus the National Cholesterol Education Program–Adult Treatment Panel III and International Diabetes Federation clinical criteria to identify high-risk men with an altered cardiometabolic risk profile. Metab. 2009; 58: 1123-1130.
- Haffner SM. Abdominal adiposity and cardiometabolic risk: do we have all the answers? Am J Med. 2007; 120: S10-S16.
- Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics- 2017 update: a report from the American Heart Association. Circulation. 2017; 135: e146-e603.
- Qiao Q, Gao W, Zhang L, et al. Metabolic syndrome and cardiovascular disease. Ann Clin Biochem. 2007; 44: 232-263.
- Moore JX, Chaudhary N, Akinyemiju T. Metabolic Syndrome Prevalence by Race/Ethnicity and Sex in the United States, National Health and Nutrition Examination Survey, 1988-2012. Prev Chronic Dis. 2017; 14: E24-E24.
- Alberti KGMM, Eckel RH, Grundy SM, et al. Harmonizing the Metabolic Syndrome. Circulation. 2009; 120: 1640-1645.
- Nolan PB, Carrick-Ranson G, Stinear JW, et al. Prevalence of metabolic syndrome and metabolic syndrome components in young adults: A pooled analysis. Prev Med Rep. 2017; 7: 211-215.
- Toms R, Bonney A, Mayne DJ, et al. Geographic and area-level socioeconomic variation in cardiometabolic risk factor distribution: a systematic review of the literature. Int J Health Geogr. 2019; 18: 1.
- Puckrein GA, Egan BM, Howard G. Social and Medical Determinants of Cardiometabolic Health: The Big Picture. Ethnic Dis. 2015; 25: 521-524.
- Cordain L, Eaton SB, Miller JB, et al. The paradoxical nature of hunter-gatherer diets: meat-based, yet non-atherogenic. Eur J Clin Nutr. 2002; 56: 1: S42.
- Drewnowski A, Popkin BM The Nutrition Transition: New Trends in the Global Diet. Nutr Rev. 1997; 55: 31-43.
- Singh RB, Takahashi T, Nakaoka T, et al. Nutrition in transition from Homo sapiens to Homo economicus. Open Nutraceuticals J. 2013; 18: 21.
- Blasbalg TL, Hibbeln JR, Ramsden CE, et al. Changes in consumption of omega-3 and omega-6 fatty acids in the United States during the 20th century. Am j Clin Nutr. 2011; 93: 950-962.
- Ruiz-Núñez B, Pruimboom L, Dijck-Brouwer DAJ, et al. Lifestyle and nutritional imbalances associated with Western diseases: causes and consequences of chronic systemic low-grade inflammation in an evolutionary context. J Nurt Biochem. 2013; 24: 1183-1201.
- Thorburn AN, Macia L, Mackay CR. Diet, Metabolites, and “Western-Lifestyle” Inflammatory Diseases. Immunity. 2014; 40: 833-842.
- Ronto R, Wu JHY, Singh GM. The global nutrition transition: trends, disease burdens and policy interventions. Public Health Nutr. 2018; 21: 2267-2270.
- Carrera-Bastos P, Fontes-Villalba M, O'Keefe JH, et al. The western diet and lifestyle and diseases of civilization. Res Rep Clin Cardiol. 2011; 2: 15-35.
- Sibai AM, Nasreddine L, Mokdad AH, et al. Nutrition Transition and Cardiovascular Disease Risk Factors in Middle East and North Africa Countries: Reviewing the Evidence. Ann Nutr Metab. 2010; 57: 193-203.
- Schmidt MD, Dwyer T, Magnussen CG, et al. Predictive associations between alternative measures of childhood adiposity and adult cardio-metabolic health. Int J Obes. 2010; 35: 38.
- Llewellyn A, Simmonds M, Owen CG, et al. Childhood obesity as a predictor of morbidity in adulthood: a systematic review and meta?analysis. Obes rev. 2016; 17: 56-67.
- Slopen N, Goodman E, Koenen KC, et al. Socioeconomic and Other Social Stressors and Biomarkers of Cardiometabolic Risk in Youth: A Systematic Review of Less Studied Risk Factors. PLoS ONE. 2013; 8: e64418.
- Scoditti E, Capurso C, Capurso A, et al. Vascular effects of the Mediterranean diet-part II: role of omega-3 fatty acids and olive oil polyphenols. Vascular pharmacology. 2014; 63: 127-134.
- Fitó M, Konstantinidou V. Nutritional Genomics and the Mediterranean Diet's Effects on Human Cardiovascular Health. Nutrients. 2016; 8: 218-218.
- Calton EK, James AP, Pannu PK, et al. Certain dietary patterns are beneficial for the metabolic syndrome: reviewing the evidence. Nutr Res. 2014; 34: 559-568.
- Rescigno T, Micolucci L, Tecce MF, et al. Bioactive Nutrients and Nutrigenomics in Age-Related Diseases. Molecules. 2017; 22: 105.
- Ordovas JM. Corella D. Nutritional genomics. Annu Rev Genomics Hum Genet. 2004; 5: 71-118.
- Johnson M, Pace RD, McElhenney WH. Green leafy vegetables in diets with a 25: 1 omega-6/omega-3 fatty acid ratio modify the erythrocyte fatty acid profile of spontaneously hypertensive rats. Lipids Health Dis. 2018; 17: 140.
- Johnson M, McElhenney WH, Egnin M. Influence of Green Leafy Vegetables in Diets with an Elevated omega-6:omega-3 Fatty Acid Ratio on Rat Blood Pressure, Plasma Lipids, Antioxidant Status and Markers of Inflammation. Nutrients. 2019; 11.
- Smith JN, Caldwell LJ, van der Merwe M, et al. A Comparison of Dietary and Caloric Restriction Models on Body Composition, Physical Performance, and Metabolic Health in Young Mice. Nutrients. 2019; 11.
- Most J, Gilmore LA, Smith SR, et al. Significant improvement in cardiometabolic health in healthy nonobese individuals during caloric restriction-induced weight loss and weight loss maintenance. Am J Physiol Endocrinol Metab. 2017; 314: E396-E405.
- Solon-Biet SM, McMahon AC, Ballard JWO, et al. The Ratio of Macronutrients, Not Caloric Intake, Dictates Cardiometabolic Health, Aging, and Longevity in Ad Libitum-Fed Mice. Cell Metab. 2014; 19: 418-430.
- Voortman T, van den Hooven EH, Tielemans MJ, et al. Protein intake in early childhood and cardiometabolic health at school age: the Generation R Study. Eur J Nutr. 2016; 55: 2117-2127.
- Johnson M, Bradford C. Omega-3, omega-6 and omega-9 fatty acids: implications for cardiovascular and other diseases. J Glycomics Lipidomics. 2014; 4: 2153-0637.1000123.
- Simopoulos AP, Leaf A, Salem Jr N. Essentiality of and recommended dietary intakes for omega-6 and omega-3 fatty acids. Ann Nutr Metab. 1999; 43: 127-130.
- Manson JE, Cook NR, Lee IM, et al. Marine n-3 fatty acids and prevention of cardiovascular disease and cancer. New Engl J Med. 2019; 380: 23-32.
- Caldera PC, Deckelbaumc RJ. CURRENT OPINION Omega-3 fatty acids and cardiovascular outcomes: an update. Curr Opin Clin Nutr Metab Care. 2018; 21: 000-000.
- Jia X, Kohli P, Virani SS. Omega-3 Fatty Acid and Cardiovascular Outcomes: Insights From Recent Clinical Trials. Curr Atheroscler Rep. 2019; 21: 1.
- Poudyal H, Panchal SK, Diwan V, et al. Omega-3 fatty acids and metabolic syndrome: effects and emerging mechanisms of action. Prog Lipid Res. 2011; 50: 372-387.
- Harris WS, Mozaffarian D, Rimm E, et al. Omega-6 Fatty Acids and Risk for Cardiovascular Disease. Circulation. 2009; 119: 902-907.
- Mathias RA, Sergeant S, Ruczinski I, et al. The impact of FADS genetic variants on omega6 polyunsaturated fatty acid metabolism in African Americans. BMC genetics. 2011; 12: 50.
- Sergeant S, Hugenschmidt CE, Rudock ME, et al. Differences in arachidonic acid levels and fatty acid desaturase (FADS) gene variants in African Americans and European Americans with diabetes or the metabolic syndrome. The British journal of nutrition. 2012; 107: 547-555.
- Simopoulos AP. Evolutionary aspects of diet, the omega-6/omega-3 ratio and genetic variation: nutritional implications for chronic diseases. Biomed Pharmacother. 2006; 60: 502-507.
- Simopoulos AP. The omega-6/omega-3 fatty acid ratio, genetic variation, and cardiovascular disease. Asia Pac J Clin Nutr. 2008; 17: 131-134.
- Hibbeln JR, Nieminen LRG, Blasbalg TL, et al. Healthy intakes of n−3 and n–6 fatty acids: estimations considering worldwide diversity. Am J Clin Nutr. 2006; 83: 1483S-1493S.
- Simopoulos AP. The importance of the ratio of omega-6/omega-3 essential fatty acids. Biomed Pharmacother. 2002; 56: 365-379.
- Chilton FH, Dutta R, Reynolds LM, et al. Precision Nutrition and Omega-3 Polyunsaturated Fatty Acids: A Case for Personalized Supplementation Approaches for the Prevention and Management of Human Diseases. Nutrients. 2017; 9: 1165.
- Serhan CN, Chiang N Van Dyke TE. Resolving inflammation: dual anti-inflammatory and pro-resolution lipid mediators. Nature reviews Immunology. 2008; 8: 349-361.
- Simopoulos AP. The Importance of the Omega-6/Omega-3 Fatty Acid Ratio in Cardiovascular Disease and Other Chronic Diseases. Exp Biol Med. 2008; 233: 674-688.
- Maruthur NM, Wang NY J. AL Lifestyle Interventions Reduce Coronary Heart Disease Risk. Circulation. 2009; 119: 2026-2031.
- Larsson SC, Tektonidis TG, Gigante B, et al. Healthy Lifestyle and Risk of Heart Failure. Circulation. 2016; 9: e002855.
- Kris-Etherton P, Fleming J, Harris WS. The Debate about n-6 Polyunsaturated Fatty Acid Recommendations for Cardiovascular Health. J Am Diet Assoc. 2010; 110: 201-204.
