Long Term Health Outcomes Following Coronary Artery Bypass Grafting: A Different Journey for Men and Women
G.M. Lindsay*, P.R. Ponaiah, I. Nomani, S.M. Lamadah, N.A. Tayyib and A. Johargy
College of Nursing, Umm Al-Qura University, Taif Road, Makkah, Saudi Arabia
Abstract
Background: The applicability of the Short Form (SF36) questionnaire to disparate populations led us to use this tool to investigate how health-related quality-of-life (HRQoL) for patients who underwent coronary artery bypass grafting (CABG) is related to gender, age and survival.
Method: SF36 data and the presence of cardiac symptoms were collected from 44 women and 166 men prior to surgery and from consenting survivors at one and eight-year follow-ups. Survival data were collected from government records for 18 years post operation. Paired t-tests, Pearson correlation coefficients, chi-squared tests and the log-rank test were used to investigate connections between HRQoL and age, presence of angina/breathlessness and survival within and across genders.
Results: HRQoL improved significantly for males and females in almost all health domains at the one year follow-up. At the eight year follow-up most female domain scores showed further improvement whereas the majority of male domain scores declined. Cardiac symptoms were present in 75.8% of women and 68.3% of men (χ2=0.7120, p=0.3988) at the one-year follow-up, and 84.2% of women and 70.2% of men at the eight-year follow-up. Male long term survival (53.6% after 18 years) depended significantly on retaining post-operative improvements in HRQoL to the medium term (p<0.002 in 4 of 8 domains). Female long term survival (40.9%) was significantly less than male survival (p=0.0108) and depended on maintaining a steady upward trend in HRQoL over the medium term. Age was not a determinant in HRQoL following CABG. Long term male and female survival was not significantly different and approached those of age and gender matched samples from the general population.
Conclusion: Strategies to improve HRQoL in women may support improved survival by reducing excess short term female mortality, but the effectiveness of the same strategy for men is less apparent.
Introduction
Coronary Artery Bypass Grafting (CABG) is a standard routinely performed revascularization procedure in the management of CHD (Coronary Heart Disease), showing results in improved longevity1. The majority of procedures are performed for patients with continued symptoms of CHD after optimal medical management. However, longer term follow-up information on symptomatic and wider health outcomes is not collected and collated routinely other than at the level of individual care management. Data in the public domain are typically 30 day mortality and numbers of hospital procedures with rates of mortality2,3. The female and male patients investigated in this work had respective 30 day mortality rates of 11.4% and 3.6%4 and are noticeably larger than more recent rates for the same procedure3. We have no further information as to why the short term female mortality is so high.
Long term data pertaining to the relative survival of male and female patients following CABG is sparse. The predominant view from the literature5-9 is that women fare worse than men following CABG, although there is some evidence to suggest that the gender gap is slowly closing8. Suggested explanations for this disparity in survival rate between the sexes are that women present at older ages with more advanced states of disease5,6,9, and that women also have, on average, more comorbidities5. These effects are potentially compounded by the smaller diameters of female coronary vessels making these more difficult to revascularise and more susceptible to the effect of narrowing than equivalent vascular damage in men10. However, contrary to the prevailing view, a 5 year study in the Emilia-Romagna region of Italy involving a comparison of two matched cohorts of 1331 female patients with a cohort of 5976 male patients found male and female survival rates to be similar11.
This work extends the temporal horizon of a cohort study which has reported previously on earlier outcomes of patients who had undergone CABG surgery4,12-15. Survival to 1st January 2014 (approximately 18 years post surgery) is reported together with health related quality of life (HRQoL) data to eight years post surgery as measured by the Short Form 36 (SF36) assessment questionnaire16. This questionnaire is recognized as a valid and reliable tool for evaluating general health status in a normal population17 and in the context of patients undergoing percutaneous transluminal angioplasty and changes in symptoms following intervention18. We have reported on its use in this cohort to assess improvements in HRQoL one year following CABG13.
The impact of CABG on HRQoL is investigated separately for male and female patients from data collect at three times pre and post surgery, and how HQRoL relates to gender, age and long term survival.
Methods
Ethical approval
Ethical approval was obtained for the initial study investigation. Approval for additional follow up of health status was gained from the Local Research Ethical Committee (LREC), Glasgow Royal Infirmary, UK, after assurance that survival status was confirmed before contacting previous participants. This was included in the study procedures4.
Short form 36
HRQoL was measured using the Short Form 36 (SF36) questionnaire developed by Ware et al.16. The questionnaire has 36 individual questions which are used to generate scores from zero to one hundred in each of eight domains of health19. Higher scores in any domain relate to better health status in that domain. The eight domains are Physical Functioning (PF, 10 Questions), Role Limitation due to physical health problems (RP, 4Q), Bodily Pain (BP, 2Q), General Health (GH, 5Q), Energy and Vitality (EV, 4Q), Social Functioning (SF, 2Q), Mental Health (MH, 5Q) and Role Limitation due to mental health problems (RE, 3Q). Each participant was sent a self-completion questionnaire prior to review and collected at the time of interview.
Methods of analysis
Paired and unpaired differences in mean SF36 domain scores were compared using Student’s t-test rejecting the Null hypothesis at the 5% level of significance. Tests comparing numbers of female and male patients used Pearson’s chi-squared test with the appropriate number of degrees of freedom and a 5% level of significance. Correlations were calculated using Pearson’s product moment coefficient using a 5% level of significance. Survival curves for female and male patients over a period of 18 year are constructed using the Kaplan-Meier estimator and these curves are compared using the Log-rank test.
Results
Study sample
The methods for the establishment of the study cohort, the assessment instruments used and the follow up procedures are reported elsewhere13. Briefly, a random sample of patients was recruited from elective surgery at approximately one month prior to operation. Three interviews were conducted: one at baseline within one month of the operation and at follow-up interviews one year and eight years post operation. Long term survival data to 18 years were collected from government records of deaths20. An initial cohort of 210 (44F,166M) underwent CABG, reducing to 199 (39F,160M) at the one year follow-up, 165 (30F,135M) at the eight year follow-up and 105 (16F,89M) after 18 years. Self-rated severities of cardiac symptoms or their presence/absence were also collected at interview.
Age profile of study participants
Patient ages were grouped in age bands of 5 years as shown in Figure 1. The fractions of women and men in each age band were tested and found not to be significantly different (χ2=1.3949, p=0.8451). Female ages range from 40.7 years to 73.7 years (58.7, SD=7.6) at the time of operation while male ages range from 39.8 years to 79.3 years (58.0, SD=7.7).
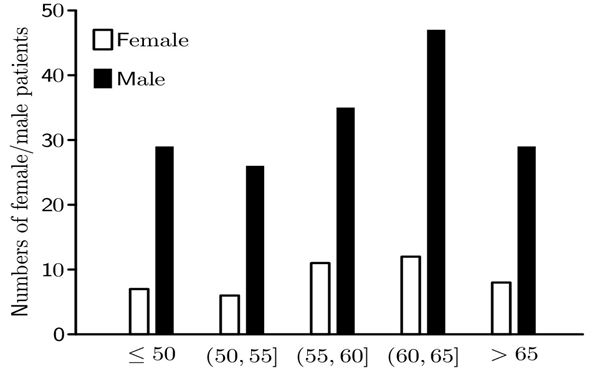
Figure 1: Histogram of the numbers of female/male (clear/solid column) patients distributed in bands of 5 years from less than 50 years to 65 years or more at the time of CABG surgery.
Figure 2 shows that mean male scores exceed mean female scores in the majority of domains at baseline and at the one year follow-up, but at the eight year follow-up this situation is reversed. However, no statistically significant differences were found at baseline, or at the one year or eight year follow-ups.
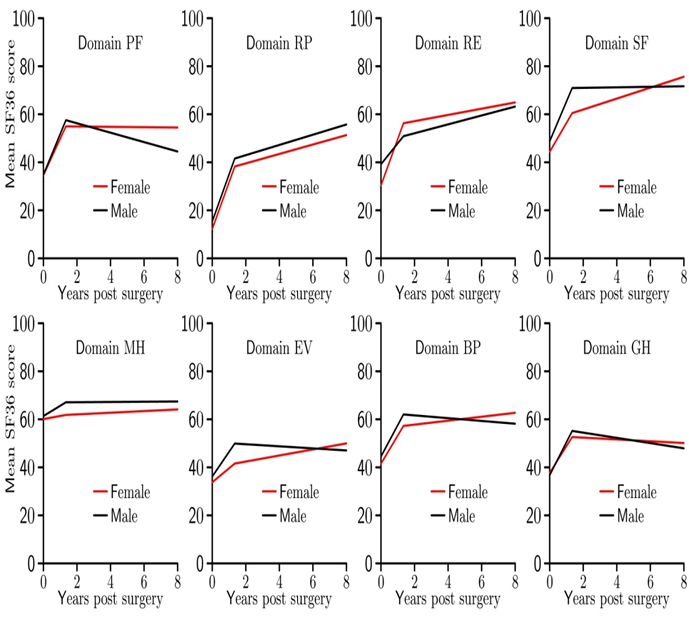
Figure 2: Mean scores for the eight health domains of SF36 at baseline, one year and eight year follow-ups are plotted for women and men.
Paired differences between health scores were calculated from fully completed SF36 questionnaires received from (44F,153M) patients at baseline, (32F,132M) patients at the one year follow-up and (19F,91M) patients at the eight year follow-up. Table 1 shows that the mean changes (paired) in domain scores for women and men between baseline and the one year follow-up are increased in all domains at the one year follow-up with the majority of improvements being statistically significant.
Table 1: Mean paired change in SF36 domain scores from baseline to the one year follow-up and from the one year to the eight year follow-up for women and men. Changes without an associated p-value are not statistically significant.
| Change in SF36 domain score from baseline to the one year follow-up | Change in SF36 domain score from the one year to eight year follow-ups | |||
|---|---|---|---|---|
| Female (p-value) |
Male (p-value) |
Female (p-value) |
Male (p-value) |
|
| PF | 15.54 (p < 0.001) |
22.47 (p < 0.001) |
-6.08 | -12.79 (p < 0.001) |
| RP | 22.79 (p = 0.004) |
26.13 (p < 0.001) |
4.69 | 11.21 (p = 0.052) |
| RE | 27.08 (p < 0.001) |
10.21 (p=0.032) |
8.33 | 13.95 (p = 0.011) |
| SF | 10.21 (p=0.051) |
20.07 (p < 0.001) |
6.94 | 0.31 |
| MH | 2.41 | 5.09 (p = 0.004) |
3.75 | -0.03 |
| EV | 3.92 | 12.56 (p < 0.001) |
8.13 | -4.59 (p = 0.034) |
| BP | 12.12 (p = 0.024) |
17.10 (p < 0.001) |
6.95 | -4.58 |
| GH | 14.96 (p = 0.002) |
18.25 (p < 0.001) |
-2.25 | -8.31 (p = 0.002) |
Women show further non-statistically significant increases in six out of eight domains and decreases in two domains between the one year and eight year follow-ups. However, for men domains RP and RE show further significant increases, 4 domains are unchanged but domains PF and EV show significant decreases. In overview, these findings suggest that female HRQoL is stable with a modest trend for improvement, whereas male HRQoL is less stable being a mixture of significant improvements in some domains and declines in others.
Correlations between age and HRQoL
Female age at baseline is significantly negatively correlated with RP and positively correlated with MH, but at one year post operation no significant correlations were found between age and domain scores. These findings suggest that older women are more physically limited at baseline, but have above average quality of mental health. The important finding, however, is that age is not a critical determinant of female HRQoL post CABG.
Male age at baseline and at the one year follow-up is positively correlated with all domains of HRQoL. In particular, the correlations with Mental Health at baseline and Energy Vitality and General Health at the one year follow-up are statistically significant. Thus the CABG intervention preferentially benefits HRQoL in older men in the short term.
Correlations between age and changes in HRQoL
The impact of surgery to a patient’s HRQoL is determined by the size and direction of the changes in their domain scores, in the short term from baseline to the one year follow-up and in the longer term from the one year to the eight year follow-ups.
No significant correlations were found between age and changes in female HRQoL scores between consecutive times of data collection. Between baseline and the one year follow up 7 of the 8 domains of HRQoL were negatively correlated with age, but 7 of the 8 correlations between age and changes in HRQoL between the one and eight year follow-ups were positive. Thus younger women initially experience greater improvements in HQRoL, but surviving older women show long term above average upward trends in their HRQoL.
Correlations of male age with the change in domain scores from baseline to the one year follow-up were mixed, but none were significant. However, 7 of the 8 correlations of male age with the change in domain scores between the one year and the eight year follow-ups were negative, and in particular the correlation with Role Physical was negative and statistically significant. Thus male age is not detrimental to the benefit of the CABG intervention, but over the longer term older men struggle to maintain early gains.
Health-related Quality of Life and Angina/Breathlessness
At baseline 41/43 women (95.3%) and 159/161 men (98.8%) suffered from angina, breathlessness or both. Although the CABG intervention reduced the severity or angina and/or breathlessness symptoms in the vast majority of patients, nevertheless cardiac symptoms persisted at the one year follow-up in 25 of 33 women (75.8%) and 99 of 145 men (68.3%). Abbate et al.21 also report a high persistence of angina following coronary revascularization with approximately 90% of patients experiencing one or more episodes of angina in the six months following surgery, and at least one third of patients experiencing several bouts of angina per week.
At the eight year follow-up a cardiac symptom was present in 16 of 19 (84.2%) women and 66 of 94 (70.2%) men. Comparisons of the presence of cardiac symptoms at baseline and the eight year follow-up are difficult because of the small numbers of female patients, but at the one year follow-up a chi-squared test comparing the presence of a cardiac symptom between women and men gave (χ2=0.7120, p=0.3988) indicating no difference in the presence of a cardiac symptom between women and men.
Correlations of female HRQoL with presence of angina/breathlessness
Correlations between female HRQoL and the presence of angina/breathlessness were negative at baseline in 7/6 out of eight domains, but none were significant. All correlations with HRQoL and the presence of angina were negative at the one year and eight year follow-ups, but again none were significant. Correlations of HRQoL and the presence of breathlessness were negative in 7 out of 8 domains at the one year and eight year follow-ups, with 2 significant correlations at the one year follow up and 5 significant correlations at the eight year follow-up. The exception was Role Emotional which correlated positively, but not significantly, with the presence of breathlessness. These findings indicate that it is the relief of breathlessness rather than angina that is the more important factor in improving the HRQoL of women.
Correlations of male HRQoL with presence of angina/breathlessness
Correlations between male HRQoL and the presence of angina/ breathlessness at baseline were negative in 7/6 out of 8 domains, but none were significant. Correlations between male HRQoL and the presence of angina/breathlessness at the one year and eight year follow-ups were all negative and significant (p<0.05). Post surgery HRQoL for men is thus dominated by the effectiveness of the CABG intervention to relieve angina and breathlessness symptoms.
Health-Related Quality of Life and Survival
Comparison of female and male survival
Female and male survival rates are compared over a period of 18 years from the date of operation using the Kaplan-Meier estimator22. Figure 3 plots the value of this estimator for the female (solid red) and male (solid blue) sample populations. The dashed red and blue lines correspond to the survival experience of a gender and age-matched cohort of the general population23.
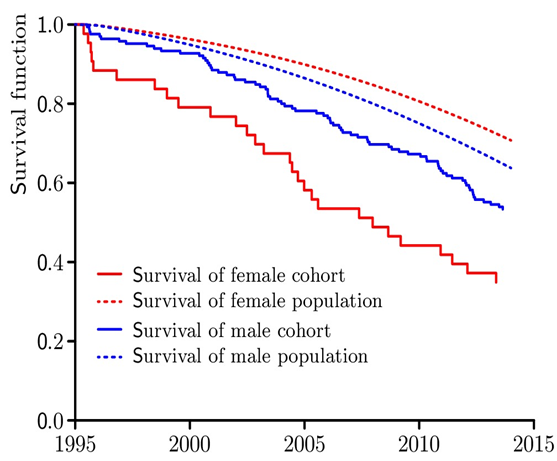
Figure 3: Survival curves (solid lines) for the male (blue) and female (red) cohorts of the study are shown together with the expected survival curves (dashed) for an age and gender matched cohort from the general public23.
Twenty eight (N=28) and seventy seven (N=77) female and male deaths respectively occurred during the period of the study. The estimated median survival for female patients was 12.97 years, and the mean survival was 12.06 years with 95% confidence interval (10,03,14.10). The mean survival for male patients was 15.02 years with 95% confidence interval (14.17,15.88), but the median survival could not be estimated because less than half of the male sample died during the period of the study. A Log-rank comparison of the Kaplan-Meier survival curves for the female and male patients gave χ2=7.1514 (p=0.0075) indicating significantly different survival risk for female and male patients over the period of the study. Figure 3 shows two periods of excess female mortality, one period immediately following CABG and a second period approximately ten years following CABG. This behaviour has also been noted in other studies24-26.
The Log-rank test applied to the Kaplan-Meier survival curves for female and male patients surviving beyond twelve years gave χ2=0.9125 (p=0.3394) indicating that survival rates for male and female patients beyond 12 years post intervention are not different, a result which agrees with the findings from other studies26,27. Figure 3 supports this result and shows long term male and female survival curves declining at approximately the same rates. Figure 3 also suggests that long term survivors of CABG experience similar mortality to that of the general population.
The relationship between HRQoL and survival
Columns 1 and 2 of Table 2 show separately the difference in mean scores at the one year follow up for women and men who survive to the eight year follow-up and those who do not. Columns 3 and 4 of the Table repeat the calculation at the eight year follow-up for patients who survive to the end date of the study and those who do not.
Table 2: Difference in mean domain scores at the one year follow-up for women/men surviving/not surviving to the eight year follow-up (cols 1,2), and at the eight year follow-up for women/men surviving/not surviving to the end date of the study (cols 3,4). Only statistically significant differences have been given an associated p-value.
| Difference in mean SF36 domain scores between surviving/not surviving female and male patients for the one year to the eight year follow-up, and from the eight year follow-up to the end date of the study | ||||
|---|---|---|---|---|
| One year follow-up for survival/not survival to the 8 year follow-up | Eight year follow-up for survival/not survival to the end date of study | |||
| Female | Male | Female | Male | |
| PF | 2.91 | 3.20 | 1.25 | 21.58 (p = 0.001) |
| RP | -0.29 | 25.95 (p = 0.005) | 13.07 | 5.38 |
| RE | -19.43 | 26.90 (p = 0.012) | 18.56 | 2.56 |
| SF | 1.01 | 3.96 | 13.61 | 23.34 (p = 0.003) |
| MH | -5.52 | 6.62 | 12.96 | 8.71 |
| EV | 11.92 | 7.60 | 10.82 | 0.77 |
| BP | -7.75 | 4.15 | 2.23 | 15.22 (p = 0.014) |
| GH | 12.97 | 5.26 | 10.33 | 13.85 (p = 0.010) |
Column 1 of Table 2 shows 4 positive and 4 negative differences, none of which are significant in the comparison of mean scores at the one year follow-up between female survivors to the eight year follow-up and those who do not. Thus short term HRQoL is unrelated to female medium term survival. Column 3 of Table 2 shows that all differences are positive but none are significant in the comparison of mean scores at the eight year follow-up between female survivors to the end date of the study and those who do not. Thus women surviving long term have, on average, better medium term HRQoL than those who do not.
Column 2 of Table 2 shows all differences are positive in the case of men, two of which are significant, between male survivors to the eight year follow-up and those who do not. Thus short term improvement in HRQoL is related to medium term survival of men. Column 4 of Table 2 shows that men surviving to the end date of the study had better HRQoL in all domains at the eight year follow-up, four of these differences being significant, than those who survived to the eight year follow-up but not to the end date of the study.
The relationship between change in HRQoL and survival
The short term and medium term benefits to HRQoL from the CABG intervention are measured respectively by the changes in domain scores from baseline to the one year follow-up and from the one year to eight year follow-ups.
Table 3: Columns 1 and 2 show the difference in the mean change in scores from baseline to the one year follow-up for female/male patients surviving/not surviving to the eight year follow-up. Columns 3 and 4 give the equivalent differences from the one year to eight year follow-ups for female/male patients surviving/not surviving to the end date of the study. P-values are shown for significant differences only.
| Difference in mean SF36 scores between surviving and not surviving female and male patients | ||||
|---|---|---|---|---|
| Change from baseline to the one year follow-up for survival/not survival to the 8 year follow-up | Change from the one year to the eight year follow-up for survival/not survival to the end date of study | |||
| Female | Male | Female | Male | |
| PF | 9.31 | 16.91 (p = 0.013) | 30.87 | -1.68 |
| RP | 2.57 | 34.84 (p = 0.003) | 47.50 | -17.97 |
| RE | 4.19 | 41.88 (p < 0.001) | 31.11 | -7.01 |
| SF | -0.78 | 17.00 (p = 0.043) | 8.15 | 12.44 |
| MH | -3.19 | 4.48 | 6.00 | 2.14 |
| EV | -6.64 | 11.06 (p = 0.018) | 21.00 | -6.57 |
| BP | 6.73 | 10.42 | 17.04 | 1.58 |
| GH | -11.48 | 4.89 | 27.07 (p = 0.010) | 1.77 |
Column 1 of Table 3 shows mixed behavior for women with 4 positive and 4 negative differences none of which are significant suggesting short term gains/losses in female HRQoL are unrelated to medium term survival for women. Column 3, however, indicates that average HRQoL of women surviving to the end date of the study was better in every domain of HQQoL, and significantly better in General Health, than women surviving in the medium term but not to the end date of the study.
Conversely, column 2 of Table 3 indicates that male eight year survival was related to higher early (one year) gains in all HRQoL domains of SF36, and statistically significantly in the domains of PF, RP, RE, SF and EV. However, column 4 of Table 3 with 4 positive and 4 negative differences indicates that male survival beyond the medium term was unrelated to gains in HRQoL over the period from the one year to eight year follow-ups.
Tables 2 and 3 taken together indicate that it is the size of the improvement in General Health rather than the domain score that is the significant marker of long term survival in women. Although only one change in domain scores is statistically significant at the eight year follow-up, nevertheless long term female survival is, on average, characterized by modest improvements in all domains of HQRoL in the short to medium term.
Tables 2 and 3 taken together indicate that male medium term survival relates to higher short term (one year) gains in HRQoL, while longer term survival is associated with retaining these short term gains to the medium term.
Discussion
This study took place in the West of Scotland which in the early years of this work was well known to have a particularly high incidence of ischaemic heart disease. During 2002 there were 494 cases and 215 deaths per 100000 men in Scotland, which at the time was the second highest rate in Western Europe28. The patients in this study were largely drawn from inner city areas, exhibited high levels of social and material deprivation and had a significant numbers of comorbidities, particularly smoking in women. Many followed a lifestyle diet of predominantly fast/processed food and low consumption of fruit and vegetables resulting in a high incidence of coronary disease mortality in both sexes, which was exceptionally high in the case of women29.
Much commentary has reported on male and female differences and experiences in CHD ranging from symptom presentation, investigation practices and outcomes of treatments including the investigation of outcomes following coronary bypass surgery. Durations of study typically divide into periods of 12 months or less24,30-36, periods of around four to five years7,11,25,37,38 and periods of eight or more years39,40 of which this study examining survival to 18 years post-operatively is an example. Briefly, the literature reports that HRQoL initially improves significantly post surgery for both genders although women experience excess mortality. The literature also reports a reduction in cardiac symptoms, particularly for men as observed in this study. Around four/five years post surgery female HQQoL is reported to be lower than that of males7. However, in the longer term no statistically significant differences in HRQoL were reported between the genders40 in agreement with the findings of Figure 2. Interestingly in Figure 2 average female HRQoL exceeded average male HRQoL in 6 out of 8 domains in this study. A possible explanation is that longer term female survival is characterized by slowly improving HRQoL domains, whereas over the same period male HRQoL is typically characterized by a significant initial improvement in post CABG followed by a slow downwards trend.
In this investigation both sexes received, on average, an immediate and significant improvement in HRQoL as a result of surgery (Table 1) in keeping with the findings of other studies10,30,36,40. On balance, female age was not a discriminatory factor with regard to HRQoL after CABG11,27,36-38. Although younger women experienced greater short term gains in HRQoL, older women showed these gains over the longer term (Sections 3.1, 3.2). On balance, male age was also not a discriminatory factor with regard to HRQoL after CABG11,27,36-38 but for the opposite reason. While older men achieved higher short term gains in HRQoL as a result of the CABG intervention, over the longer term these same patients struggled to retain these gains (Sections 3.1, 3.2). A general finding also reported by other authors7,33,35 is that, on average, female HRQoL scores and female gains in HRQoL as a outcome of CABG both lie below those for men in most domains of HRQoL.
A previous investigation showed that women and men experience similar levels of angina and breathlessness13. The small numbers of female patients free of cardiac symptom at baseline and the eight year follow-up made gender comparisons difficult, but the finding in this work was that women had a significantly higher incidence of cardiac symptoms than men at the one year follow-up.
Section 4 indicates that the presence of these cardiac symptoms is particularly detrimental to male HRQoL, a finding that is also reported in the literature24. In this study all domains of male HRQoL were significantly negatively correlated with angina and/or breathlessness, whereas the equivalent correlations for women, although negative, were weaker (Section 4).
Figure 3 indicates that short to medium term survival rates were significantly lower for women than men in this study, a finding which has been reported by a number of authors11,25-27,34,38,41. Specifically, women experience different cardiac symptoms from men supporting the view that their cardiac health could be considered to be subjectively different42. An important contributing factor is thought to be the smaller diameters of coronary vessels in women making them more difficult to revascularise and more susceptible to the effect of narrowing than would be the case for equivalent vascular damage in men. Although the incidences of hypertension for women (79.5%) and men (86.3%) in this study were not statistically different (p=0.2899), the presence of hypertension in women is thought to magnify their susceptibility to coronary events by comparison with similar levels of hypertension in men10. Also women tend to present coronary symptoms at a later age than men resulting in an increased urgency of coronary procedure10,25,27,37, although this explanation does not apply to the women in this study. As commented previously, Figure 3 indicates that the long term slopes of the survival curves for both genders are not greatly different suggesting that the long term survival rates for both genders are similar26,27; the increased female mortality occurs in the short to medium term post operation. A long term study of survival following bypass surgery noted increased mortality 8-10 years post intervention41. Figure 3 shows this effect for women, although here it may be an artifact of a small sample. The same effect is not apparent for men.
Tables 2 and 3 show that medium term female survival was not significantly related to short term gains in HRQoL, but women who improved their HRQoL over the medium term had better long term survival prospects. On the other hand, men surviving to the medium term had significant initial improvements in HRQoL, but their longer term survival was correlated with retaining these early gains in HRQoL to the medium term. Beyond 12 years male and female survival is not different and indeed Figure 3 suggests that it is similar to that of the general population.
Personal health monitoring in combination with cohort surveillance and developments in the digital world will increase one’s ability to collect even richer real-time data. However, time must still elapse in order to allow the long term consequences and outcomes of interest following major healthcare interventions to be revealed.
Conclusion
The primary finding of this work is that women initially experience smaller improvements than men in HRQoL from CABG but have an upwards trajectory over the medium term. On the other hand men tend to show the reverse behavior with initially significant improvements in HRQoL which they struggle to retain over the longer term. Strategies to improve HRQoL in women may support improved survival by reducing excess short term female mortality, but the effectiveness of the same strategies for men is less apparent.
Acknowledgement
The initial phase of this study was undertaken as a research training fellowship funded by the Chief Scientist Office, Scottish Office, Department of Health, Scotland. The cohort follow-up studies were funded by the Chief Scientist Office, Scottish Office, Department of Health, Scotland, reference number 31560, CZH/4/44.
References
- Taggart DP. CABG or stents in coronary artery disease: end of the debate? The Lancet. 2013; 381(9867): 605–607.
- Bridgewater B. Cardiac registers: the adult cardiac surgery register. Heart. 2010; 96: 1441-1443.
- National Audit, Cardiac Surgery Audit report data 2010/11. https://data.gov.uk/dataset/813153dc-66b9-4049-a968-a603cd7f2ef2/national-adult-cardiac-surgery-audit-report-data-2010-11/datafile/1a6cebb7-9415-4bef-bc6c-469cd54b9224/preview Accessed 16th Jan, 2019.
- Lindsay GM. The health and well-being of individuals before and after coronary artery bypass surgery. PhD Thesis University of Glasgow Library. 1998.
- Blankstein R, Ward RP, Arnsdorf M, et al. Female gender is an Independent predictor of operative mortality after coronary artery bypass graft surgery. Circulation. 2005; 112: I-323-I-327.
- Guru V, Fremes SE, Austin PC, et al. Gender differences outcomes after hospital discharge from coronary artery bypass grafting. Circulation. 2006; 113(4): 507-16.
- Gijsberts CM, Agostoni P, Hoefer IE, et al. Gender differences in health-related quality of life in patients undergoing coronary angiography. Open Heart. 2015; 2: e000231. doi:10.1136/openhrt-2014-000231.
- Swaminathan RV, Feldman DN, Pashun RA, et al. Gender differences in in-hospital outcomes after coronary artery bypass grafting: long-term results. Journal of Cardiothoracic Surgery. 11: 144. DOI 10.1186/s13019-016-0538-4.
- Mokhles MM, Soloukey Tbalvandany S, Siregar S, et al. Male-female differences in aortic valve and combined aortic valve/coronary surgery: a national cohort study in the Netherlands. Open Heart. 2018; 5: e000868. doi:10.1136/openhrt-2018-000868.
- Mikhail GW. Coronary revascularisation in women. Heart. 2006; 92(Suppl III): iii19–iii23. doi: 10.1136/hrt.2005.070359.
- Nicolini F1,2, Vezzani A3, Fortuna D, et al. Gender differences in outcomes following isolated coronary artery bypass grafting: long-term results. Journal of Cardiothoracic Surgery. 2016; 11: 144 DOI 10.1186/s13019-016-0538-4.
- Lindsay GM, Smith LN, Hanlon P, et al. Coronary heart disease patients’ perception of their health and expectations of benefit following coronary artery bypass grafting. J Advanced Nursing. 2000; 32: 1412-1421.
- Lindsay GM, Hanlon P, Smith LN, et al. Assessment of changes in general health status using the short-form 36 questionnaire 1 year following coronary artery bypass grafting. Eur J Cardio-thorac Surg. 2001; 18: 557-564.
- Lindsay GM, Tolmie EP, Martin WM, et al. Smoking after Coronary artery Bypass; high early follow up mortality. Thoracic and Cardiovascular Surgeon. 2009; 57: 135-140.
- Belcher PR, Gaw A, Cooper M, et al. Are we negating the benefits of coronary artery bypass grafting? Journal of Human Hypertension. 2002; 16: 691-697.
- Ware JE Jr, Snow KK, Kosinski AS, et al. SF-36: Health Survey Manual and Interpretation Guide. Boston Mass Nimrod Press. 1993.
- Jenkinson C, Coulter A, Wright L. Short form 36 (SF36) health survey questionnaire: normative data for adults of working age. Brit Med J. 1993; 306: 1437-40.
- Krumholz HM, McHorney CA, Clark L, et al. Changes in health after elective percutaneous coronary revascularization. A comparison of generic and specific measures. Med Care. 1996; 34: 754-759.
- Rand Health: 36-Item Short Form Survey (SF36) Scoring Instructions. https://www.rand.org/health/surveys_tools/mos/36-item-short-form/scoring.html (Accessed 14th Dec 2018).
- National Records of Scotland https://www.nrscotland.gov.uk/research/guides/statutory-registers/deaths Accessed 18th December, 2018.
- Abbate A, Biondi-Zoccai GGL, Agostoni P, et al. Recurrent angina after coronary revascularization: a clinical challenge European Heart Journal. 2007; 28: 1057–1065 doi:10.1093/eurheartj/ehl562.
- Goel MK, Khanna P, Kishore J. Understanding survival analysis: Kaplan-Meier estimate. Int J Ayurveda Res. 2010; 1(4): 274–278. doi:10.4103/0974-7788.76794.
- Office for National Statistics, 2018. National life tables for Scotland. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/lifeexpectancies/datasets/nationallifetablesscotlandreferencetables
- Penckofer S, Ferrans CE, Fink N, et al. Quality of Life in Women Following Coronary Artery Bypass Graft Surgery. Nursing Science Quarterly. 2005; 18(2): 176-183.
- Filardo G, Hamman BL, Pollock BD, et al. Excess short-term mortality in women after isolated coronary artery bypass graft surgery. Open Heart. 2016; 3: e000386. doi:10.1136/openhrt-2015- 000386.
- Veena G, Fremes SE, Tu JV. Time-related mortality for women after coronary artery bypass graft surgery: A population-based study. The Journal of Thoracic and Cardiovascular Surgery. 2004; 1158-65.
- Al-Alao BS, Parissis H, McGovern E, et al. Gender influence in isolated coronary artery bypass graft surgery: a propensity match score analysis of early outcomes. Gen Thoracic Cardiovascular Surgery. 2012; 60(7): 417-24. doi: 10.1007/s11748-012-0082-7.
- Mitchell R, Fowkes G, Blane D, et al. High rates of ischaemic heart disease in Scotland are not explained by conventional risk factors. Journal of Epidemiology and Community Health. 2005; 59: 565-67 doi: 10:1136/jech.2004.029850.
- The Scottish Monica Project. https://thl.fi/publications/morgam/cohorts/full/uk/unk-sco.htm
- Rantanen A, Tarkka MT, Kaunonen M, et al. Health-related quality of life after coronary artery bypass grafting. Journal of Advanced Nursing. 2009; 65(9): 1926–36. doi: 10.1111/j.1365-2648.2009.05056.x.
- Lavdaniti M, Tsiligiri M, Palitzika D, et al. Assessment of Health Status Using SF-36 Six Months after Coronary Artery Bypass Grafting: A Questionnaire Survey. Health Science Journal. 2015; 9: 1-7.
- Taghipour HR, Naseri MH, Safiarian R, et al. Quality of Life One Year after Coronary Artery Bypass Graft Surgery. Iranian Red Crescent Medical Journal. 2011; 13(3): 171-77.
- Lindquist R. Dupuis G. Terrin M, et al. Comparison of health-related quality-of-life outcomes of men and women after coronary artery bypass surgery through 1 year: findings from the POST CABG Biobehavioral Study. Am Heart J. 2004; 146(6): 1038-44.
- Arif R, Farag M, Gertner V, et al. Female Gender and Differences in Outcome after Isolated Coronary Artery Bypass Graft Surgery: Does Age Play a Role? PLoS ONE. 2016; 11(2): e0145371. doi:10.1371/journal.pone.0145371.
- Koch CG, Khandwala F, Cywinski JB, et al. Health-related quality of life after coronary artery bypass grafting: A gender analysis using the Duke Activity Status Index. The Journal of Thoracic and Cardiovascular Surgery. 2004; 284-95.
- Kurfirst V, Mokrá?ek A, Krupauerová M, et al. Health-related quality of life after cardiac surgery – the effects of age, preoperative conditions and postoperative complications. Journal of Cardiothoracic Surgery. 2014; 9: 46. http://www.cardiothoracicsurgery.org/content/9/1/46
- Albilasi TM, Albilasi BM, Alonazi MA, et al. Assessment and Evaluation of the Quality of Life of Saudi Patients Underwent Coronary Artery Bypass Graft (2-5 years). The Egyptian Journal of Hospital Medicine. 2018; 70(3): 452-7.
- den Ruijter HM, Haitjema S, van der Meer MG, et al. Long-term outcome in men and women after CABG; results from the IMAGINE trial. Atherosclerosis. 2015; 241: 284-88.
- Stenvall H, Tierala I, Räsänen P, et al. Long-term clinical outcomes, health-related quality of life, and costs in different treatment modalities of stable coronary artery disease. European Heart Journal – Quality of Care and Clinical Outcomes. 2017; 3: 74–82. doi:10.1093/ehjqcco/qcw024.
- Takousi MG, Schmeer S, Manaras I, et al. Health-Related Quality of Life after Coronary Revascularization: A systematic review with meta-analysis. Hellenic Journal of Cardiology. 2016; 57: 223-237.
- Adelborg K, Horváth-Puhó E, Schmidt M, et al. Thirty-Year Mortality after Coronary Artery Bypass Graft Surgery. Circulation: Cardiovascular Quality and Outcomes. 2017; 10 (5): e002708. DOI: 10.1161/CIRCOUTCOMES.116.002708
- Fogoros RN. (2018). How Cardiac Symptoms are Different in Women. www.verywellhealth.com/cardiac-symptoms-in-women-1745822 Accessed 28th Jan, 2019.
