Pleuropericardial Cyst: A Review of the Literature
Christina Koumantzia, Nikolaos Saridakis, Andreas Eleftheriou*
Department of Neurology, and Department of Clinical and Experimental Medicine, Linköping University, Linköping, Sweden
Abstract
Background: Pleuropericardial cysts (PPCs), account for 5 - 10% of all mediastinal tumours, are rare lesions occurring in approximately 1 in 100000 persons and are usually congenital and rarely acquired. They are detected post-mortem or incidentally on routine chest X-ray (CXR) and in most cases multi detector Computer Tomography is used to confirm the diagnosis. As benign course and clinical latency are characteristic features of such cysts and the occurrence of complications is rare, the majority of them can be left untreated.
Methods: The aim of the study is to review the literature regarding PPCs and create a table which summarises all the published cases in order to draw a conclusion about the epidemiology, as well as the diagnostic and therapeutic approach to PPCs exclusively. We reviewed retrospectively the clinical manifestation, diagnostic and therapeutic approach in 101 cases of PPCs since the 19th century.
Results: Our statistical analysis led to the following results: mean age of initial detection: 48.7 ± 17.2 years, female:male ratio: about 3:2, presence of symptomatology: 37/101 cases, most common location: right cardiophrenic angle (RCPA), most common method of initial detection: CXR in 49/101 cases, mean maximal diameter: 8,3 ± 3 cm.
Conclusion: The management of a pleuropericardial cyst should be based on an algorithm in which the cyst's size, shape and compressibility along with clinical presentation and patient's fitness and preferences are be taken into consideration. When interventional is required, surgical resection by means of traditional open surgery or minimally invasive methods are considered to be the gold standard and along with percutaneous aspiration are the methods that have mostly been used.
Introduction
Pleuropericardial cysts, account for 5 - 10% of all mediastinal tumours, are rare lesions occurring in approximately 1 in 100000 persons and are usually congenital but exceptionally acquired. They are detected post-mortem or incidentally on routine chest X-ray and in most cases multi detector Computer Tomography is used to confirm the diagnosis. As benign course and clinical latency are characteristic features of such cysts and the occurrence of complications is rare, the majority of them can be left untreated.
Cystic lesions surrounding the heart have been reported since 18541. The first published pathoanatomic case series including four diverticula and one cyst was completed in 19032. Kienböck described the radiographic appearances of what may have been a pericardial coelomic cyst and later enriched this description by introducing the differential diagnosis of pleuropericardial cysts3,4. Otto Pickhardt was the first to delineate the thoracoscopic appearance and later proceeded to the resection of a pericardial coelomic cyst in a 53-year-old woman5. Symptoms coexisting with such cysts were first described by Freedman and Simon, D'Abreu and Churchill and Mallory. Reviewing the literature, it was Adrian Lambert who was the first to propose a pathogenesis, noting the similar embryological origin of PPCs and diverticula from disconnected mesenchymal lacunae which normally fuse to develop the pericardial coelom. He also attempted for the first time to differentiate the thin-walled cysts of the mediastinum, all of which had previously been reported as "probably of lymphatic origin"6. Greenfield et al. introduced the term "Spring water cyst"7. By 1958, at least 120 cases of mesothelial cysts had been reported8,9.
PPCs are cyst walls made up of a single layer of mesothelial cells and a loose stroma of fibrous tissue with collagen and elastic fibres. They usually contain clear, serous fluid and that is why they are also called ‘spring water’ cysts10. Finally, both the expression of epithelial membrane antigen and calretinin and the absence of an actin-positive subepithelial smooth muscle layer may be helpful in the diagnosis of a PPC11.
The aim of this study was to review the literature and present a review article about PPCs including a table with all the data of: a) all the published cases reported as "pleuropericardial cysts" in the title and b) some of the published cases described as "pericardial cysts" in the title which are also called "pleuropericardial cysts" either in other review articles or even in the same article. According to our knowledge, this is the first organized attempt to review whole literature with focus in PPCs.
Finally, we analysed statistically the data associated with the age of initial detection, gender and cyst size and location, in order to draw a conclusion regarding the epidemiology of PPCs exclusively.
Methods
We aimed to review the literature regarding PPCs and create a table which summarises all the published cases in order to draw a conclusion about the epidemiology, as well as the diagnostic and therapeutic approach of PPCs exclusively.
We first searched the PubMed and Medline databases for any publications concerning PPCs. After this we searched for a systematic review reporting PPCs. No systematic reviews were found. We found only a review of treatment of four cases with video-thoracoscopy. We also found a review for benign cysts of the mediastinum. We then independently searched PubMed (until February 2018) using the following free text terms: “pleuropericardial cyst”, "pleuropericardial cyst" AND “treatment” OR “symptoms” OR “location” OR “intervention” OR “surgery” OR “case”. Then we searched for pericardial cysts also. We included case reports, abstracts, editorials and articles in all languages describing the location or symptoms or treatment or intervention or surgery in patients with PPC. The database created from the electronic searches compiled in a reference manager program (Endnote X8) and all duplicated citations was eliminated. The following data were collected: (1) publication details such as title, authors, and other citation details, (2) patient data such as age, sex, symptoms (3) details of PPC (location, size, and approval), (4) data of intervention or surgery, (5) follow-up data. All in all, we reviewed 139 publications and found 101 cases of PPCs.
As described in “Discussion”, plenty of terms have been used to describe a PPC. So, review references are mostly based on the terms "pericardial" and "pleuropericardial" and we decided to include the following in table 1:
1) All the published cases referred as "pleuropericardial cysts" in the title.
2) All the published cases referred as "pericardial cysts" in the title which are called "pleuropericardial cysts" either in other review articles or even in the same article but later on, in the text.
After having collected the data from all the cysts referred as PPCs (101 cases from 47 publications), we carried out an univariate statistical analysis regarding the following parameters: age of initial detection, gender, cyst size and location, method of initial detection as well as presence of symptomatology. Cases with non-mentioned data were excluded from the analysis.
Results
As far as the mean age of initial detection is concerned, our statistical analysis showed that this was approximately 48.7 ± 17.2 years, ranging from 3 to 76 years in 50 cases out of 101. Regarding gender, the female:male ratio was calculated to be about 3:2 (29:21) among 50 cases, while the most frequent location was the right cardiophrenic angle (RCPA) accounting for 39,6% followed by the left (LCPA) at 18,9% among 53 patients. CXR was the method used for initial detection in 49/101 cases. The percentage was probably higher, as the method for initial detection was not mentioned in 41 cases. Symptomatology was present in 37 cases out of 101. Finally, the mean maximal diameter was 8.3 ± 3 cm, varying between 1.5 and 17 cm in 42 out of 101 patients.
Discussion
Plenty of terms have been employed in the literature to characterise PPCs. Most have been used to define the localisation, the contents, the histology or the pathogenesis of such cysts. These terms are: pericardial coelomic cysts6, pericardial cysts, hydrocele of the mediastinum, simple cyst of the mediastinum, serosal cyst, spring- or clear- water cyst7, para-pericardial cyst, pleuropericardial cyst, pleural cyst and mesothelial mediastinal cyst.
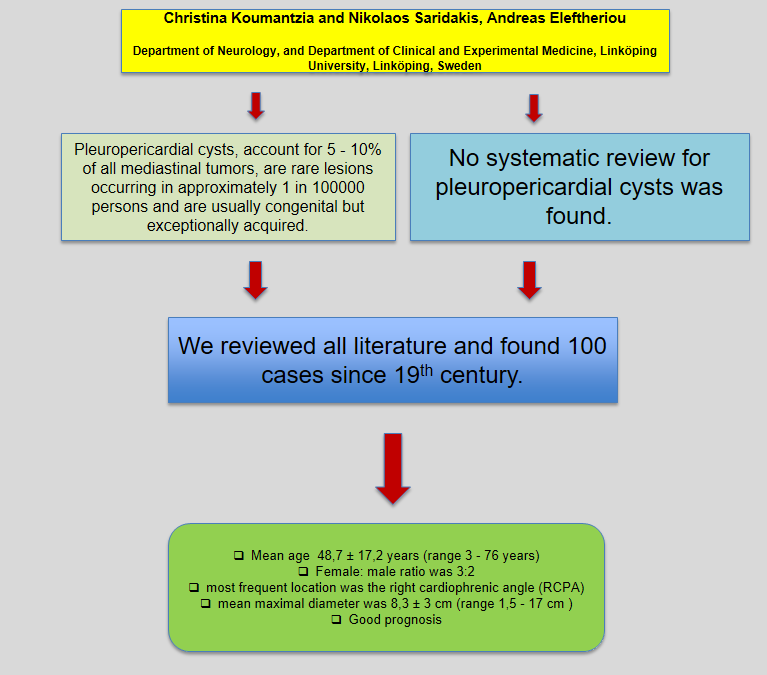
Figure 1:
PPCs are usually congenital in origin but other causes such as inflammation (rheumatic pericarditis, bacterial infection particularly tuberculosis, echinococcosis), trauma, post cardiac surgery and chronic haemodialysis12-17 have been reported. Congenital PPCs usually originate from failure of fusion of one of the mesenchymal lacunae that form the pericardial sac, during embryogenesis after the third week of gestation6,18. Another theory of the pathophysiology of such cysts explains the origin of PPCs by means of differential perseverance and graded constriction of ventral recess of the pericardial coelom. The ventral parietal recess is a diverticular structure where most of PPCs are located. Perseverance of this structure forms the diverticulum, constriction of the proximal part of which results in either a diverticulum with a narrow neck or a PPC in communication with the pericardial cavity, while the complete closure of the proximal recess gives rise to a PPC1. As far as inflammatory cysts are concerned, they develop as a result of loculated pericardial effusion12.
PPCs account for 5-10% of mediastinal tumours and 11%2 or 30%4,5 of mediastinal cysts. Prevalence is approximately 1 in 100000 persons8 and they constitute the second most common type of primary mediastinal cysts after bronchial ones19,20. All ages may be affected, but PPCs are most frequently identified between the third and fifth decade of life, while they are rarely detected in childhood21-24. More specifically, less than 20 cases in children have been reported in the literature25. As far as gender is concerned, the female: male ratio varies among many studies and it has been described to be 1:122, 8:426 and 2:38. Finally, PPCs can be associated with other diseases such as Fanconi anaemia27,28.
PPCs can occur in any compartment of the mediastinum29, but are usually detected in the visceral mediastinum30,31 attached to the parietal pericardium. The most frequent site is the right cardiophrenic angle (51-75%), followed by the left (28-38%)19-21,32,33. Those PPCs occurring elsewhere other than the cardiophrenic angles (8% - 16%) are usually superior to the heart and right–sided34. A frequent site is the right latero-tracheal region35. In this case, the cyst originating from the upper recess of the pericardium extends posteriorly from the pericardial cavity around the ascending aorta36,37. Other unusual sites that have also been reported include the other two mediastinal compartments, the vascular hila, the subcarinal area and the left heart border33,38-42. Moreover, the PPCs that are detected in locations remote from the pericardium are believed to be pedunculated with a stalk that connects them with the pericardium43,44. Almost 5% of PPCs are in communication with the pericardium through determinable tube-like structures45. However, others studies indicate that they are always attached to the pericardium directly or by a pedicle10,19,20, although a visible connection between the cyst and the pericardium is rarely detected46,47. Finally, a PPC may occasionaly present as a mobile chest lesion, described by the term "wandering PPC"48 and in this case, it should be differentiated from solitary fibrous tumours of the pleura, which are the most common mobile chest masses49.
PPCs usually have a diameter of 2-15cm44,50-52 and weigh 100-200gr25. However, there have been reported cases up to 28cm53or even larger containing 1300ml of fluid34 or measuring 25x37x5cm54, while other were as large as a grapefruit55.
The majority of PPCs are asymptomatic (50-75%) in adults and are found post-mortem or incidentally on routine CXR38,56. However, two thirds of children diagnosed with a PPC develop symptomatology8.When they are symptomatic, in general due to increasing size and consequent compression or invasion on nearby organs, the symptoms are generally dominated by respiratory signs, such as dyspnoea, stridor, wheezing, chest discomfort including vague chest pain, heaviness, retrosternal pressure or substernal pain, persistent cough, sputum, haemoptysis, dysphagia and epigastric pain. Circulatory signs such as tachycardia, palpitations, fatigue, cyanosis and weakness may also be found8,19,31,44,47,50,57-61,62. There can also appear signs of nervous compression presented as hoarseness due to unilateral vocal cord paralysis as a result of left recurrent laryngeal nerve compression63, hemidiaphragm paralysis, hiccups, intercostal neuralgia, Horner Syndrome and Pancoast Tobias Syndrome64. Finally, PPCs can atypically herniate through the chest wall and become palpable on clinical examination13.
Table 1: Presentation of all data concerning 101 cysts referred as "pleuropericardial cysts" in the literature.
| No of Reference | Year | No of PPCs | Age (y) of initial detection | Sex | Symptoms Clinical presentation | Method for initial detection | Initial Suspicion | CT | MRI | Location | Size (cm) | Indication for further intervention | Follow up time |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BIlal et al. | 2017 | 17 | NM | NM | NM | NM | NM | NM | NM | NM | NM | NM | NM |
| Naqvi et al. | 2016 | 1 | 24 | M | Exertional dyspnea (NYHA II), occasional cyanosis over the lips, loud P2 with 4/5 murmur in early and midpart of systole best heard in the auscultation position of pulmonary valve (pulmonary stenosis) | CXR | PPC | Large PPC with significant stenosis of main pulmonary artery + few subcentrimetric mediastinal lymph nodes | NP | LAM | NM | Symptomatic and complicated cyst | NM |
| Mouroux et al. | 1996 | 13 | Mean age: 49.9 (range 22-75) | 4M 9F | -7/13: symptomatic -Chest pain presented as the most common symptom in 5/7 patients due to cyst infection (1/5) or because of herniation of the cyst (1/5) | 13/13: CXR | NM | -11/13: 1-10 HU density -2/13: 38 and 52 HU density. -13/13: No contrast uptake | Performed in 5/13 because of paravertebral position (2/5), abnormal density on CT (2/5) or herniation through the chest wall (1/5) but results are NM. | -5/13:RCPA -3/13:LCPA -2/13:R parathacheal space -2/13: Paravertebral mediastinum -1/13:Anterior mediastinum | Mean diameter: 7.5(±4) X 5(±2) | -7/13: Symptomatic cysts -3/13: Uncertain diagnosis -2/13: Compression on the SVC, although asymtpomatic -2/13: Practice of a potentially traumatic sport or professional activity | -Mean observation time via CXR: 57.7 mo, (range 4-125) -6/13: >72 mo follow up -No recurrence along with absence of symptoms |
| Arghir et al. | 2013 | 1 | 62 | F | Progressive exertional dyspnea, night sweats, L chest pain, minor reccurent hemoptysis, tachycardia and hypertension | CXR | Heart disease (PPC after TTE) | Smooth ovoid thin-walled, sharply defined, homogenous mass(without tear drop configuration) | NP | LCPA | 10x11 | Symptomatic cyst and uncertain diagnosis | 1 mo AT via CXR: LVH, ascended left hemidiaphragm |
| Elatiqi et al. | 2015 | 1 | 52 | F | R basithoracic pain for 6 months described as burning, impaired general status | CXR | NM | Well-limited, fluid density cystic lesion | NP | RCPA | NM | Symptomatic cyst and uncertain diagnosis | 5 w AT via CT: tuberculoid adenitis (+chest pain) |
| Kang et al. | 2010 | 1 | 49 | M | Pain on the right hemithorax for 2 days, after physical exertion, worsened with movement and during inhalation | CXR | -Pulmonary embolism -PPC after CT | Well-defined, ovoid cyst filled by fat tissue and dense linear structures in its mid-anterior view ("whirl sign": torsion) | NP | RCPA | 17x12,5 | Symptomatic and complicated with torsion cyst | NM |
| Nitu et al. | 2017 | 1 | 52 | F | Chronic cough, night sweats, progressive exertional dyspnea, weight loss, pallor and diminished breath sounds on the L lower lung area. | CXR | Encysted pleurisy | Encysted pleural effusion | NP | LCPA | 5x8 | Initial size and possible complications (but the patient refused surgery) | 6 mo AD via CT: no growth of the remaining cyst |
| Boisserie-Lacroix et al. | 1988 | 1 | 45 | M | NM | CXR | Bronchogenic cyst or PPC | Rounded mass of water density | T1: intermediate signal indensity, T2:increased signal indensity | R Latero-tracheal position | NM | RIsk of fissuration | NM |
| Sandeep Krishna Nalabothu et al. | 2015 | 1 | 43 | M | Exertional dyspnoea, pain in the R anterior chest | CXR | NM | Cystic mass | NP | RCPA | 8x6 | None | "regulargly" (NM) |
| Arthur et al. | 1997 | 1 | 66 | M | Intermittent chest discomfort unrelated to exertion for several mo, bilateral 2+ pitting pedal edema, hypertension, 3/4 systolic murmur and RBBB without RVH | TTE | NM | NP | Irregular mass of muscle density compressing the free wall of RV | Mass adjacent to the heart anteriorly | 10x6 | Symptomatic cyst and uncertain diagnosis | 1 mo AT via TTE: no RV outflow tract obstruction along with resolution of symptoms and clinical signs |
| Prachi et al. | 2006 | 1 | 61 | F | Asymptomatic | CXR | PPC | Well-defined, unilocular cystic mass adjacent to IVC and attached to the pericardium by a pedicle | NP | RCPA | NM | None | 3 mo AD via CT: migration of PPC in the interval into the right major fissure |
| Ochsner et al. | 1966 | 11 | NM specifically | NM specifically | 10/11: Asymptomatic 1/11: Dyspnea and frequent episodes of substernal pain | CXR | NM | NP | NP | Symptomatic cyst: RCPA Other cysts: NM | Symptomatic cyst's diameter: 12 Other cysts' size: NM | 1/11: Symptomatic cyst | -NM specifically -Generally: no recurrence |
| Parienty et al. | 1984 | 1 | 13 | F | Asymptomatic | CXR | PPC | Homogeneous mass with low attenuation and no contrast uptake | NP | RCPA | NM | Growth of the cyst (observed after 12 y) | Lost to follow up for 12 y. 1 y AT (26 y old) via CXR: normal |
| Juneja et al. | 2017 | 2 | A,B: 65 | A,B: F | A: Non productive cough, exertional dyspnea and R sided dull aching chest pain B: Persistent non productive cough for 1 y | A: TTE B: CXR | A: Encysted empyema B: D/D: 1.Cardiomegaly 2.L pleural effusion 3.L lower lobe mass | A,B:Fluid density lesions without significant contrast uptake (B:large and well-defined) | A,B: NP | A: RCPA B: LCPA | A: 7x4x1,5 B: 10x3.4x5.5 | A:NM (but the patient refused surgery) B: NM (but the surgery was deferred in view of the high risk) | A,B: NM |
| Swain et al. | 2016 | 1 | 68 | M | Hoarseness for 2 mo, L vocal cord paralysis (= L RLN paralysis) | Neck and thorax CT | Giant PPC | Giant, smooth ovoid mass with a thin, slightly higher density wall and low density contents | NP | LAM (+ middle mediastinum) extending downwards from the thoracic inlet | NM | Symptomatic and complicated cyst | 6 mo AT via NM method (completely asymptomatic patient) |
| Mitu et al. | 2017 | 1 | 71 | F | Palpitations, vertigo, impaired general status, altered mental status, amnesia, hypotension, SR with extrasystoles | Abdominal Ultrasound | PPC | Oval, well defined, homogenous lesion without contrast uptake and signs of local aggresiveness | NP | Retrocardiac in relation to IVC and esophagus | 3x2.5 | None | NM |
| Lozano et al. | 2010 | 1 | 62 | M | Asthenia, anorexia, itchy and dry cough, retrosternal pressure. Complicated with progressive dyspnea, orthopnea, oppressive chest pain (cardiac tamponate) | CXR | PPC | Thin-walled cyst, partial atelectasis | NP | LAM adjacent to the border of the heart and large vessels | 12.1 × 10.1 ×14 | Symptomatic and complicated cyst (hemodynamic instability) | NM |
| Adil et al. | 2010 | 1 | 68 | M | Dyspnea NYHA I associated with stridor (airway compression) and chest pain in the left upper thoracic wall for 3 mo | CXR | PPC | Large well-defined cystic mass, adjacent to the aortic arch, pulmonary trunk and L pulmonary artery and pushing the L lung downwards | NP | LCPA extending superiorly to the apical pleural cavity and medially to the lung hilum | 9x7x8 | Symptomatic cyst | 1 mo AT via CXR: normal |
| El Hammoumi et al. | 2014 | 1 | 35 | M | Moderate dyspnea for 4 months associated with fever and mucous excretions | CXR | NM (opacity of water density) | Pericardial effusion in a tick-walled cystic cavity | NP | Right paratracheal region | NM | Symptomatic and complicated with cardiac tamponade cyst, uncertain diagnosis and prevention of further complicatons | 1 mo and 8 mo via CT: complete recovery and no recurrence |
| Bava et al. | 1998 | 1 | 8 | M | Chest pain, muffled cardiac tones, sinus tachycardia (110bpm), slight ST-segment elevation in inferior and anterior leads | TTE | PPC | NP | Pedunculated pericardial mass originating in the upper mediastinum | LCPA | 9x10 | Uncertain diagnosis and onset of signs of cardiac tamponade | 4-year AT follow up via CXR and TTE: no recurrence |
| Yeste et al. | 2017 | 1 | 51 | M | Fever, arthralgia and weight loss | CXR | Infected PPC | Mass consistent with infected embryonic remnants | NP | LAM (+ middle mediastinum) | 9x7 | Symptomatic and complicated with infection cyst, unusual anterior position | NM |
| Smahi et al. | 2010 | 1 | 54 | F | Exertional dyspnea and chest pain | CXR | PPC | Dumbbell shaped cystic mass surrounding the heart and great vessels | NP | Located bilateral in superio-anterior and middle mediastinum | -R portion: 14x9,5x15 -L portion: 8x4x12 | Symptomatic and large-sized cyst | 6 mo AT via (probably) CXR: No recurrence |
| Portillo-Carroz et al. | 2006 | 1 | 55 | F | Chest pain | CXR | PPC | Cystic lesion with no definable wall and no contrast uptake | NP | RCPA | Largest diameter: 6 | None | NM mo AD (''regularly'') via TTE: no significant findings |
| Beroukhim et al | 2011 | 1 | 5 | M | NM | NM | NM | NM | Smoothwalled and well-defined cyst with heterogenous appearance, T1, T1 + fat sat, MDE: Iso/Hypo-intense FPP: Hypointense SSFP: Hyperintense T2: strongly hyperintense | RCPA | Largest dimension: 6.3 | NM | NM |
| Chaturvedi et al. | 2017 | 1 | 3 | F | Fever, Swelling all over the body (anasarca), pallor, tachypnea, tachycardia, firm hepatomegaly | CXR | Fulminant hepatic failure | Cyst missed. Only suggestive of a large pericardial abscess | NP | Arround the pericardium | NM | Persistent symptomatology | NM |
| Francese et al. | 1991 | 1 | 41 | M | NM (history of thyroid papillary Ca) | Post-therapy radioiodine TBS | Metastatic lymph node | Performed but the results are NM. | Abnormal retrosternal mass | L precordial region | 3.5x5.5 | Exclusion of metastasis | NM |
| Changping Jia et al. | 2014 | 1 | 76 | F | NM (history of thyroid follicular Ca) | Post-therapy radioiodine TBS | -NM initially (probably metastasis) -PPC after CT | Round, well-defined cyst-like soft tissue nodule | NP | RCPA | 1x1.5 | None | NM mo AD via CT and radioiodine TBS: no change |
| Hermens et al. | 2001 | 3 | A:35 B:43 C:71 |
A:M B,C: F | A: Chest pain for several years B: NM (probably nothing associated with the mass) C: Paroxysmal collapse, SVC syndrome |
A,B,C: CXR | A:A cyst B:PPC C: Retrosternal goitre |
A:Homogeneous content and water density B: Cystic formation C: Large cystic formation with water density |
A,B,C: NP | A: LCPA B: RCPA C: R paratracheal position |
Maximal diameter: A: 9.5 B: 9.8 C: 10 |
A,C: symptomatic cyst B: NM |
A: 3 mo AT B: 48 mo AT C: 22 mo AT A,B,C: via CXR A,B,C: No recurrence |
| Mouroux et al. | 2003 | 4 | A: 37 B: 37 C: 51 D: 22 |
A: F B: F C: F D: H |
A: Dyspnea B: Hypochondriac pain C: Fever D: Asymptomatic |
A,B,C,D: NM | A,B,C,D: NM | A,B,C,D: NM | A,B,C,D: NM | A: RCPA B: RCPA C: LCPA D: LAM |
A: 6x3 B: 15x6 C: 6x4 D: 5x5 |
A,B,C: symptomatic cyst D: unusual location |
NM |
| Lang-Lazdunski et al. | 2008 | 1 | 72 | F | NM | NM | NM | NM | NM | NM (According to imaging: RCPA) | Diameter: 9 | NM specifically | 21 mo AT via NM method: no recurrence |
| Melfi et al. | 2012 | 9 | ΝΜ specifically | NM specifically | NM | NM specifically (In general CXR and CT was used as pre-operative evaluation) | NM specifically | NM | NM | NM specifically | -NM specifically -Mean diameter of all included mediastinal lesions: 3.1 Ranging from 1.6 to 4.2 | NM | 3 mo AT via CXR and 6 mo and 12 mo AT via CT: No recurrence |
| Department of Veterans Affairs | 2008 | 1 | NM exactly | M | Asymptomatic (psychiatric patient) | NM | NM | NM | NM | NM | NM | NM (BUT the patient refused surgery) | NM |
| Mabille et al. | 1980 | 1 | NM | NM | Sudden onset of unilateral chest pain | CXR | PPC | NM | NP | NM | NM | Symptomatic cyst | NM |
| Khan Arfa | 2005 | 1 | NM | NM | NM | CXR | NM | Performed but results are NM | NP | NM (According to imaging: LAM + superior mediastinum) | NM | NM | NM |
| Verslegers et al | 2012 | 2 | NM | NM | NM | Breast MRI | NM | NM | T2: high signal intensity | NM | NM | NM | NM |
| Halkic et al. | 2002 | 1 | 67 | M | Exertional dyspnea, dry cough and signs of left-sided pleural effusion | CXR | PPC | Extracardiac mass filled with fluid | NP | Left pericardial | 9x7 | Symptomatic cyst | 6 w AT via CXR: normal, asymptomatic patient |
| Ubeda et al. | 2009 | 1 | 72 | F | Increasing dyspnea for 2 mo, typical chest pain with effort, lower limb edema, jugular venous distension, pulmonary rales, 3cm hepatomegaly and atrial fibrillation | TTE | -Heart failure -PPC after CT | Giant PPC collapsing LV, RA and surrounding parencyma | NP | NM (according to CT images: dumbbell shaped surrounding the heart) | NM ("giant") | Symptomatic cyst | NM |
| Pun et al. | 2002 | 6 | NM | NM | NM | NM | NM | NM | NM | NM | NM | NM (athough all resected) | NM |
| Traibi et al. | 2012 | 3 | NM specifically | NM | NM specifically | -NM specifically -1/3 cases: CXR | NM | -NM specifically -1/3 cases: Cystic mass | NP | -NM specifically -1/3 cases: RCPA | NM specifically | -NM specifically -Uncertain diagnosis and symptomatic cyst generally | -NM specifically -3/3: No recurrence |
| Bacha et al | 2015 | 1 | 50 | M | Chest pain for 2 years | CT | NM | Cystic lesion | NP | Left superio-posterior mediastinum | Maximum diameter: 3,7 | Uncertain diagnosis, atypical location and symptomatic cyst | 3 y AT: asymptomatic patient |
| Eleftheriou et al. | 2019 | 1 | 37 | F | Dyspnea, Palpitations | CXR | Intermediate pneumonia | Cystic lesion (PPC) without pathologically enlarged lymph nodes and pleural effusion | NP | RCPA | 5,5x5x 6cm | None | 5y AD: asymptomatic patient |
The course of PPCs is usually benign as they are well-limited lesions with scant vascularisation. No cases of malignant degeneration have been reported in the literature. However, cases of concomitant neoplasias and PPCs and even PPCs infiltrated by neoplasias in the context of tumor progression have been described65. Self-resolution of a PPC probably due to rupture has also been reported in a few cases14,61,66-69.
Complications
The mediastinum is a narrow non-extendable space. Consequently, every mediastinal mass, including PPCs, can compress adjacent organs and this can even occasionally lead to complications as well as life-threatening emergencies9,14,37,58,64,70,71.
Table 2: All reported complications in the literature divided into 3 categories (complications due to compression, inflammatory and other complications).
| References | Compression of adjacent structures | Inflammatory complications | Other complications |
|---|---|---|---|
| Koch et al., Shaver et al | Cardiac compression | ||
| Martins et al., Shaver et al., Lesniak-Sobelga et al. | Cardiac compression of right side of heart with deviation of septum | ||
| Kruger et al. | Diastolic dysfunction, congestive heart failure, mitral valve prolapse | ||
| Antonini-Canterin et al. | Pulmonary artery stenosis, ventricular outflow tract obstruction, cardiogenic shock | ||
| Bandeira et al., Borges et al., El Hammoumi et al. | Cardiac tamponade | ||
| King et al., Padder et al. | Cyst intra-pericardial rupture | ||
| Elatiqi et al. | Spontaneous (because of quick expansion) or post-traumatic intra-cystic hemorrhage | ||
| Kang et al., Bava et al. | Torsion of the cyst's intrapericardial pedicle | ||
| Davis et al. | Lung compression and more specifically right main stem bronchus obstruction | ||
| Forouzandeh et al., Luketich et al. | Atelectasis and obstructive pneumonia | ||
| Blegrad et al. | Airway compression | ||
| Blegrad et al., Kaul et al. | Obstructive syndromes include superior vena cava syndrome | ||
| Arghir et al | Azygos vein syndrome, thoracic duct syndrome and inferior vena cava compression | ||
| Hoque et al., Yeste et al., Chopra et al., Mastroroberto et al. | Cyst infection or inflammation with or without erosion of the cyst into adjacent structures, such as the right ventricular wall or the superior vena cava | ||
| Komodromos et al. | Sepsis, pericarditis | ||
| Ilhan et al. | Pleural effusions, recurrent syncope | ||
| Vlay et al. | Atrial fibrillation | ||
| Fraser et al. | Mesothelioma | ||
| Fredman et al. | Sudden death |
Diagnostic approach-Differential diagnosis
The diagnostic approach to PPCs is based on the clinical presentation and the results of imaging studies. However, the fact that PPCs may be clinically and radiologically similar to other mediastinal lesions makes the diagnosis challenging. The location and nature of mediastinal lesions are very important for the differential diagnosis. Differential diagnosis of PPCs is quite wide and includes not only lesions found in the middle mediastinum where PPCs are most commonly identified, but also lesions occurring in the other two mediastinal compartments9,11,29,72-76.
Table 3: Differential diagnosis of PPCs including lesions that can be found in any mediastinal compartment, as particularly for large lesions it may be difficult to define their origin.
| 1. Congenital cysts of primitive foregut origin (bronchogenic cyst, enterogenic cyst and esophageal duplication cysts) | 17. Lymphomas |
| 2. Broncial cysts | 18. Mesenchymal tumors (sarcomas44, hemangiomas and lymphangiomas133) |
| 3. Localised pericardial or pleural effusion9 | 19. Right middle lobe pathology |
| 4. Ventricular aneurysms or aneurysms of the ascending aorta | 20. Morgagni hernia |
| 5. Fluid-filled superior aortic recess134 | 21. Hiatus hernia |
| 6. Prominent left atrial appendage | 22. Diaphragmatic hump |
| 7. Varicose pericardial vein135 | 23. Diaphragmatic tumors |
| 8. Epicardial fat pad | 24. Cystic degeneration of mediastinal tumors133 |
| 9. Lipoma | 25. Metastatic and bronchogenic carcinoma44 |
| 10. Hydatid heart disease / Echinococcal cysts | 26. Granulomatous lesions44 |
| 11. Thymic masses (thymic cyst, thymoma, thymolipoma, thymic lymphoma, thymic carcinoid) | 27. Mediastinal abscesses44 |
| 12. Thyroid diseases (retrosternal goiter, thyroid adenoma) | 28. Thoracic duct cysts136,137 |
| 13. Parathyroid cysts (very rarely) | 29. Neurogenictumors (neurofibroma, cysticschwannoma) |
| 14. Germ cell tumors (dermoid cyst, mature teratoma, malignant teratoma, seminoma) | 30. Meningoceles104,137 |
| 15. Hattori's cyst / Mullerian cyst138 | 31. Mediastinal located pancreatic pseudocyst |
| 16. Enlarged lymph nodes with cystic necrotic degeneration133,139 |
A CXR can localise as well as identify PPCs by means of posterior-anterior and lateral views. However, a disadvantage of this method is the fact that it cannot provide much information about the morphology and the expanse of the lesion. Further imaging studies such as MDCT, MRI, ultrasonography, angiography and positron emission tomography (PET) scan are used in order to complement and corroborate the initial diagnosis or suspicion40,58,77.
With CXR, PPCs are demonstrated as teardrop formations on the lateral views as the cysts tend to adjust to the medial aspect of the pulmonary fissure. Furthermore, this projection can depict the alteration in shape and the movable nature of fluid-filled PPCs, during respiration or postural changes41,51,64,78,79,80. In postero-anterior projection, PPCs usually appear as rounded or oval opaque shadows with uniform density and well-defined borders and without calcification77. PPCs can also take on different and unusual radiologic appearances, such as a dumbbell shape20,28,81.
MDCT with or without contrast remains the gold standard for further investigation of a mediastinal mass14. It estimates the size and nature of the mass, defines its position within the mediastinum and how it is related to the adjacent structures, providing valuable information about its morphology as well as its extent82,83. On a CT scan, the PPC is a thin-walled, well-marginated, oval homogeneous mass, usually unilocular, while multilocular cysts have also been reported8. Their attenuation is low (0-20HU), although sometimes it may be a little higher than water density (30-40 HU). This is probably because of a high protein and cells content due to bleeding or infection84. As they are commonly avascular25, they are not enhanced with contrast agents46,85. Other atypical CT findings include the presence of calcification, a sharp upper border25,44,86 and the presence of associated pericardial effusion. Moreover, MDCT can show stalks connecting PPCs to the pericardium, thus a certain diagnosis can be established even for PPCs in unusual locations48,87-93. PPC torsion can also get depicted via a CT scan as a mass of soft tissue in which there is an internal intertwine with fat and soft tissue attenuation, called the ''whirl sign’' which was first described in intestinal volvulus28,94,95.
Two-dimensional echocardiography was first used in order to detect a pericardial cyst96. Transthoracic and in some cases transoesophageal echocardiography is a superior noninvasive method, which can accurately depict the PPC's position and distinguish it from other possible diagnoses (solid tumours, fat pads, coronary, ventricular or aortic aneurysms)14,20,96. Ultrasonographically PPCs appear typically as homogeneous anechoic thin-walled masses29,67. Transoesophageal echocardiography can be helpful especially for PPCs in unusual locations and in case of haemodynamic compromise in order to confirm a suspected compression of the large vessels or the cardiac cavities97,98. Finally, ultrasonography can set the diagnosis of PPCs prenatally beyond the 14th week of gestation99.
MRI is similar to CT as far as the efficacy in detecting a tumour is concerned100. MRI is a useful tool for both the initial diagnosis of a mediastinal mass and the post-therapeutic follow-up. It gives a better anatomical depiction of PPCs, including those in atypical locations and their relationships to adjacent structures, including blood vessels, without the use of contrast material20. Thus, it is helpful in differentiating PPCs from vascular anomalies such as aortic aneurysms37,101,102. MRI findings are diagnostic, showing a smooth-walled and well-defined structure with high signal intensity on T2-weighted images, low-to-intermediate signal intensity on T1-weighted images and no enhancement after intravenous contrast administration85,93,103,104. High signal intensity is rarely seen on T1-weighted images in the case of high protein content20. Furthermore, MRI should be the method of choice with children and infants104.
Arteriography provides help in defining whether the lesion in question is a part of a vascular structure105. In cases where diagnosis remains challenging, cyst puncture and sequent injection of a contrast material for diagnostic and therapeutic reasons has been used106. Finally, two incidentally detections of PPCs by means of I131 total body scan due to the uptake of I131 through the pericardial serosa have been reported107,108.
Therapeutic approach
The management of all mediastinal cysts can vary from conservative follow-up, percutaneous aspiration with or without ethanol, minocyclin or doxycyclin injection to surgical treatment by means of interventional thoracoscopy or thoracotomy43,109,110,146. PPCs are commonly asymptomatic and most of them can be left without treatment. So, in the case of an asymptomatic patient and undoubted radiological diagnosis of a PPC, conservative management with cautious follow-up by means of non-contrast-low-dose CT or ultrasound or MRI is advised38,70,98,111. Although there are no specific guidelines concerning either the duration or the frequency of the follow-up and the information about safety is poor, it is widely suggested to take into consideration the patient's (new symptoms, complications) as well as the cyst's (size) stability in order to decide how to continue the management. The longest described follow-up lasted 25 years and eventually a 2.5L cyst was resected52. Treatment is indicated in the case of symptomatic, large-sized asymptomatic cysts, uncertain diagnosis and possibility of malignant potential, atypical location such as close to large vessels, high density on CT, or the presence of complications. Such treatment is required in order to prevent life-threatening emergencies such as airway and/or haemodynamic impairment, or patient's concern23,32,40,41,112-114. Thus, any anterior mediastinal lesion should be considered potentially malignant and should be surgically excised as soon as possible115.
Surgical excision of the cyst has been considered the gold standard of management especially in complicated cases with excellent outcomes98,116. It is worthy noting that although cardiopulmonary bypass is not usually required for PPCs removal, it should be on standby, mainly in case of possible cardiac compression, erosion of the right ventricular free wall or if extensive cardiac manipulation is required41. Partial cyst resection is also recommended in the case of tight adhesions to the nearby structures116. Apart from traditional open surgery, resection of mediastinal masses including PPCs has been carried out successfully by VATS or VATS with mini-thoracotomy since 199226,32,111,117-122. These minimally invasive procedures reduce surgical trauma and postoperative pain compared to open surgery leading to a shorter period of recovery and hospitalisation123,124. Furthermore, the Harmonic Scalpel which is an ultrasonically activated scissor, is recommended for performing VATS more quickly125. However, VATS also has limitations especially for removing anterior and upper mediastinal lesions4,122,126-128 giving only a limited view of the area of interest. In addition, thoracoscopy should be an option for treatment only in the case of well-encapsulated and <6cm sized masses, although successful resections via VATS on larger ones have been reported52,111,126. Robotic surgery using the da VinciTM Robotic System is another minimally invasive therapeutic modality which has proved to be safe and useful, but its cost remains a strong limitation129. Taking into consideration the above, small-to-moderate sized and typically located PPCs could be safely and successfully removed by these modern surgical procedures.
Percutaneous aspiration of the PPC contents by a thin needle puncture under ultrasound or CT guidance has been used for both diagnosis and therapy12,84,106,110. However, complications such as vascular injury, pneumothorax, anaphylaxis, and infection have been referred and recurrence in about one third of patients has been recorded57,110,130-132. Thus, percutaneous aspiration of such cysts must be performed only in case of comorbidities that contraindicate surgery, when there is a need for temporary decompression before the removal of a large symptomatic cyst9,12,133, when there is a suspicion of a tubercular PPC in order to confirm the diagnosis preoperatively13 or when a patient refuses surgery.
To sum up, the management of PPCs is based on an algorithm. The cyst's size, shape and compressibility along with clinical presentation and the patient’s fitness and preference should be taken into consideration so that the appropriate management can be chosen9.
Prognosis
The absence of symptomatology is an indicative sign of good prognosis14, while post-resection prognosis is excellent with low rates of morbidity and mortality87,98. Only one case of recurrence after excision has been documented78.
Limitations
After reviewing the literature and attempting to statistically analyse the data from table 1 we identified the following limitations:
1. Regarding the nomenclature and the classification of mesothelial cysts, plenty of terms have been used to describe a PPC. Thus, review references are mostly based on the terms "pericardial" and "pleuropericardial" and the inclusion criteria are mentioned in “Methods”. That may have affected our results as some cysts which are referred to with a different term have been excluded.
2. We had to exclude many cases from the pool of PPCs as there were not specific data with regard to the examined parameters.
3. We chose to calculate the mean maximal diameter as an objective measurable feature of size. However, our result concerning this parameter may be biased and overestimated, given that our pool of cases of cysts with known size consisted mainly of symptomatic cysts (30 out of 42 patients) which are generally supposed to be larger.
Conclusion - Recommendations
PPCs are rare and usually clinically silent, but can occasionally cause life threatening complications. The majority of them are congenital due to developmental deficits and are most commonly found incidentally via routine radiography between the third and fifth decade of life. In this study, we found out that the mean age of initial detection is roughly 48.7 years, the mean maximal diameter is 8.3 cm and the female:male ratio is approximately 3:2, which is in line with the literature. The RCPA constitutes the most common location, according to our statistical analysis.
MDCT is recommended as the method of choice in all cases, while cardiac MRI can be useful when diagnosis is more challenging.
The management algorithm of PPCs can be divided into two main categories, based on whether there is symptomatology or not. The presence of symptoms depends on the cyst’s size and eventual compression of the mass.
1. In the case of a small asymptomatic PPC that does not cause compression, follow-up with serial transthoracic echocardiography is recommended.
2. Apart from the symptomatic and/or complicated and/or large PPCs, surgery is also recommended in the case of an initially asymptomatic PPC which grows in size. This is in order to prevent complications and life-threatening emergencies. The patient’s concern constitutes a relative indication for surgical management9.
Surgical resection by means of traditional open surgery or minimally invasive methods is considered to be the gold standard, and this along with percutaneous aspiration are the methods that have mostly been used. Percutaneous aspiration and ethanol sclerosis is recommended for large symptomatic PPCs while the patient is waiting for surgery.
List of abbreviations used
PPCs: Pleuropericardial cysts; CXR: Chest X-ray; MDCT: multi detector Computer Tomography; CT: Computed Tomography; MRI: Magnet Resonance Imaging; ER: Emergency Room; VATS: Video-assisted thoracoscopic surgery.
Authors' contributions
Andreas Eleftheriou, Nikolaos Saridakis and Christina Koumantzia were the major contributors in writing the manuscript.
References
- LILLIE WI, McDONALD JR, CLAGETT OT. Pericardial celomic cysts and pericardial diverticula; a concept of etiology and report of cases. J Thorac Surg. 1950; 20(3): p. 494-504.
- AR. Ueber divertikel-und cystenbildung am perikard [in German]. Prag Med Wochschr. 1903; 28: p. 461–464.
- WM Y. Cyst of the pericardium. Am Heart J, 1931; 6: p. 710-712.
- R., K., Brit. J. Radiol. 1927. 32: p. 352.
- OC P. Pleuro-diaphragmatic cyst. In: Transactions of the New York Surgical Society-Stated Meeting held April 1, 1933. Ann Surg. 1933; 99: p. 814-816.
- AV L. Etiology of thin-walled thoracic cysts. 1940; (10): p. 1-7.
- Greenfield LSL. Touroff AS. Spring water cyst of the mediastinum. J Thorac Surg. 1943; 12: p. 495-502.
- Le Roux BT. Pericardial coelomic cysts. Thorax 1959; 14(1): p. 27-35.
- Kar SK GT, Dasgupta S. Pericardial Cyst: A Review of Historical Perspective and Current Concept of Diagnosis and Management. Interv Cardiol J. 2015; 1(1)
- Priola SM, Priola AM, Cardinale L, et al. The anterior mediastinum: anatomy and imaging procedures. Radiol Med. 2006; 111(3): p. 295-311 DOI: 10.1007/s11547-006-0031-6.
- Takahashi Y OH, Yoshifuku S, Otagiri N, et al. A Case of Müllerian Cyst Arising in the Posterior Mediastinum. ???????. 2014; 39(4): p. 804-807.
- Maisch B, Seferovi? PM, Risti? AD, et al. Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology. Eur Heart J. 2004; 25(7): p. 587-610 DOI: 10.1016/j.ehj.2004.02.002.
- Naqvi SE BM, Ali E. Tubercular pleuropericardial cyst presenting with symptomatic pulmonary stenosis. Saudi Surg J. 2016; 4: p. 37-40.
- Patel J, Park C, Michaels J, et al. Pericardial cyst: case reports and a literature review. Echocardiography. 2004; 21(3): p. 269-72 DOI: 10.1111/j.0742-2822.2004.03097.x.
- Pugliatti P, Donato R, Crea P, et al. Image Diagnosis: Pericardial Cyst in a Dialysis Patient. J Cardiovasc Ultrasound. 2016; 24(2): p. 177-8 DOI: 10.4250/jcu.2016.24.2.177.
- Saldana Duenas C, Hernandez Galan A. Posttraumatic pericardial cyst. An Sist Sanit Navar. 2015; 38(3): p. 475-8.
- Sharifi Mood B, ANR Eazadi M. Cystic tubercular pericarditis a rare form. J Res Med Sci 2005; (10): p. 2368.
- Murray JFaN, JA. Textbook of respiratory medicine. 1994: W.B. Saunders Company. 2146-2147.
- Moschos C, Kalomenidis I, Roussos C, et al. A 35-year-old male with chronic cough. Eur Respir J. 2007; 29(3): p. 608-11 DOI: 10.1183/09031936.00099706.
- Ozturk E, Aparci M, Haholu A, et al. Giant, dumbbell-shaped pericardial cyst. Tex Heart Inst J. 2007; 34(3): p. 386-7.
- Duwe BV, Sterman DH, Musani AI. Tumors of the mediastinum. Chest. 2005; 128(4): p. 2893-909. DOI: 10.1378/chest.128.4.2893.
- Mohsen SMH, Samad EJG. Pericardial Cyst Presented as Chronic Cough: A Rare Case Re-port. .Tanaffos. 2012; 11(4): p. 60-62.
- Mouroux J, Venissac N, Leo F, et al. Usual and unusual locations of intrathoracic mesothelial cysts. Is endoscopic resection always possible? Eur J Cardiothorac Surg. 2003; 24(5): p. 684-8.
- Zambudio AR, Lanzas JT, Calvo MJ, et al. Non-neoplastic mediastinal cysts. Eur J Cardiothorac Surg. 2002; 22(5): p. 712-6.
- Elatiqi Khaoula BH, Zaghba Nahid, Yassine Najiba. An operated pleuro pericardial cyst with an unusual presentation and evolution. Sch J Med Case Rep. December 2015; 3(12): p. 1167-1171.
- Alar T, Bayram AS, Gebitekin C. Pericardial cysts: an analysis of 12 cases. J Laparoendosc Adv Surg Tech A. 2011; 21(7): p. 595-8 DOI: 10.1089/lap.2011.0034.
- Balci YI, Tavil B, Akinci D, et al. Diaphragmatic mesothelial cyst in a child with Fanconi aplastic anemia. J Pediatr Hematol Oncol. 2007; 29(12): p. 860-1 DOI: 10.1097/MPH.0b013e318159e6d2.
- Kang DW, Corpa MC, Racy Mde C, et al. Pleuropericardial cyst torsion: case report. Einstein Sao Paulo. 2010; 8(2): p. 228-31 DOI: 10.1590/S1679-45082010RC937.
- Jeung MY, Gasser B, Gangi A, et al. Imaging of cystic masses of the mediastinum. Radiographics. 2002; 22 Spec No: p. S79-93 DOI: 10.1148/radiographics.22.suppl_1.g02oc09s79.
- Gürsoy S OA, Ucvet A, Erbaycu AE. Lesiones quísticas primarias y benignas del mediastino en el adulto: espectro clínico y tratamiento quirúrgico. Arch Bronconeumol. 2009; 45: p. 371-5.
- Teece PM FE, Kuhlman JE. CT evaluation of the anterior maediastinum: Spectrum of disease. Radiographics, 1994; 14: p. 973-90.
- Le Pimpec-Barthes F, Cazes A, Bagan P, et al. [Mediastinal cysts: clinical approach and treatment]. Rev Pneumol Clin. 2010; 66(1): p. 52-62 DOI: 10.1016/j.pneumo.2009.12.009.
- McAllister HA Jr. Primary tumors and cysts of the heart and pericardium. Curr Probl Cardiol. 1979; 4(2): p. 1-51.
- Shields TWLJI, Ponn RB, Rusch VW. General thoracic surgery: 166 - Overview of Primary Mediastinal Tumors and Cysts. 6th ed. 2005, Philadelphia: Lippincott Williams & Wilkins.
- Mills NL. Pericardial cyst in the superior mediastinum. Br J Radiol. 1959; 32: p. 554-6 DOI: 10.1259/0007-1285-32-380-554.
- Aronberg DJ, Peterson RR, Glazer HS, et al. The superior sinus of the pericardium: CT appearance. Radiology. 1984; 153(2): p. 489-92 DOI: 10.1148/radiology.153.2.6484182.
- Boisserie-Lacroix M, Martigne C, Laurent F, et al. A pleuropericardial cyst in an unusual location: the value of magnetic resonance. Comput Med Imaging Graph. 1988; 12(5): p. 277-80.
- Arghir OC, Dantes E, Velescu L, et al. Giant left-sided pleuropericardial cyst, mimicking a heart disease. Pneumologia. 2013; 62(1): p. 34-6.
- Patel BK, Markivee CR, George EA. Pericardial cyst simulating intracardiac mass. AJR Am J Roentgenol. 1983; 141(2): p. 292-4 DOI: 10.2214/ajr.141.2.292.
- Sandeep Krishna Nalabothu SUM, Sumalatha Chittiboyina, Kumar Varma. Pleuro Pericardial Cyst: An Incidental Finding. International Journal of Medical and Health Research. 2015; 1(2): p. 32-34.
- Ng AF, Olak J. Pericardial cyst causing right ventricular outflow tract obstruction. Ann Thorac Surg. 1997; 63(4): p. 1147-8.
- Yuncu G, Cakan A, Ors Kaya S, et al. Atypically located pericardial cysts. J Cardiovasc Surg Torino. 2001; 42(2): p. 275-8.
- Cangemi V. Pericardial cysts of the mediastinum. J Cardiovasc Surg Torino. 1999; 40(6): p. 909-13.
- Feigin DS, Fenoglio JJ, McAllister HA, et al. Pericardial cysts. A radiologic-pathologic correlation and review. Radiology. 1977; 125(1): p. 15-20 DOI: 10.1148/125.1.15.
- le Roux BT, Kallichurum S, Shama DM. Mediastinal cysts and tumors. Curr Probl Surg. 1984; 21(11): p. 1-77.
- Komanapalli PSM. Pericardial Cyst. 2014.
- Patel S, Hajmedi P, Fischbein J. Common symptoms with rare entity: a giant pericardial cyst. Am J Med. 2015; 128(10): p. e27-8 DOI: 10.1016/j.amjmed.2015.05.043.
- Agarwal PP, Seely JM, Matzinger FR. Wandering pleuropericardial cyst. J Comput Assist Tomogr, 2006; 30(2): p. 276-8.
- Karabulut N, Goodman LR. Pedunculated solitary fibrous tumor of the interlobar fissure: a wandering chest mass. AJR Am J Roentgenol. 1999; 173(2): p. 476-7 DOI: 10.2214/ajr.173.2.10430157.
- Fraser RSMN, Colman N, Paré PD. Masas situadas de manera predominante en el compartimento mediastínico anterior. Diagnóstico de las enfermedades del tórax. . 4th ed. 2002, Buenos Aires: Buenos Aires: Editorial Médica Panamericana S.A.
- Ochsner JL, Ochsner SF. Congenital cysts of the mediastinum: 20-year experience with 42 cases. Ann Surg. 1966; 163(6): p. 909-20.
- Satur CM, Hsin MK, Dussek JE. Giant pericardial cysts. Ann Thorac Surg. 1996; 61(1): p. 208-10 DOI: 10.1016/0003-4975(95)00720-2.
- Braude PD. Giant pericardial cyst. Aust N Z J Surg. 1990; 60(8): p. 640-1.
- Lam CR. Pericardial celomic cysts. Radiology. 1947; 48(3): p. 239-43 DOI: 10.1148/48.3.239.
- Leigh TFaW, HS, The Mediastinum., ed. C.C. Thomas. 1959, Illinois: Springfield.
- Juneja M, K.C., Keny S, Lawande D., Cardiophrenic Angle Opacity: A Diagnostic Dilemma. International journal of science and research. 2017; 6(3).
- De Roover P, Maisin J, Lacquet A. Congenital pleuropericardial cysts. Thorax. 1963; 18: p. 146-50.
- Hekmat M, Ghaderi H, Tatari H, et al. Giant Pericardial Cyst: A Case Report and Review of Literature. Iran J Radiol. 2016; 13(1): p. e21921 DOI: 10.5812/iranjradiol.21921.
- Kaiser LR. Thoracoscopic resection of mediastinal tumors and the thymus. Chest Surg Clin N Am. 1996; 6(1): p. 41-52.
- Masood AM, Ali OM, Sequeira R. A hiding in the lining: painful pericardial cyst. BMJ Case Rep. 2013; 2013 DOI: 10.1136/bcr-2013-008618.
- Najib MQ, Chaliki HP, Raizada A, et al., Symptomatic pericardial cyst: a case series. Eur J Echocardiogr. 2011; 12(11): p. E43 DOI: 10.1093/ejechocard/jer160.
- Andreas Eleftheriou, Nikolaos Saridakis, Christina Koumantzia; submission date 2019-02-08; Pneumonia reveals a huge pleuropericadial cyst: a Case Presentation; under review for European Journal of Medical Case Reports.
- Swain SKPJ, Mohapatra SSG, Sahu MC. Giant pleuropericardial cyst: An unusual cause of hoarseness. J Taibah Univ Med Sc. 2016; 11(5): p. 489-491.
- Mitu FMA, Ivan M, Mitu O, et al. Pleuropericardial cyst – Case report. Rev Med Chir Soc Med Nat Ia?i. 2017; 121(1).
- Lozano PMOE., Manchín CP. Cardiac Tamponade due to a Pleuropericardial Cyst with Invasive Lung Cancer. 2010; 46: 12(658-659).
- Ambalavanan SK, Mehta JB, Taylor RA, et al. Spontaneous resolution of a large pericardial cyst Tenn Med. 1997; 90(3): p. 97-8.
- Bernasconi A, Yoo SJ, Golding F, et al. Etiology and outcome of prenatally detected paracardial cystic lesions: a case series and review of the literature. Ultrasound Obstet Gynecol. 2007; 29(4): p. 388-94 DOI: 10.1002/uog.3963.
- Kruger SR, Michaud J, Cannom DS. Spontaneous resolution of a pericardial cyst. Am Heart J. 1985; 109(6): p. 1390-1.
- Martins IM, Fernandes JM, Gelape CL, et al. A large pericardial cyst presenting with compression of the right-side cardiac chambers. Rev Bras Cir Cardiovasc. 2011; 26(3): p. 504-7.
- Adil A, Hashmani S, Khan GU. Pleuro pericardial cyst. J Coll Physicians Surg Pak. 2010; 20(10): p. 685-6 DOI: 10.2010/JCPSP.685686.
- Kumar Paswan A, Prakash S, Dubey RK. Cardiac tamponade by hydatid pericardial cyst: a rare case report. Anesth Pain Med. 2014; 4(1): p. e9137 DOI: 10.5812/aapm.9137.
- Crowe JK, Brown LR, Muhm JR. Computed tomography of the mediastinum. Radiology. 1978; 128(1): p. 75-87 DOI: 10.1148/128.1.75.
- Franquet T, Lecumberri F, Joly M. Hydatid heart disease. Br J Radiol. 1984; 57(674): p. 171-3 DOI: 10.1259/0007-1285-57-674-171.
- Modic MT, Janicki PC. Computed tomography of mass lesions of the right cardiophrenic angle. J Comput Assist Tomogr. 1980; 4(4): p. 521-6.
- Strollo DC, Rosado-de-Christenson ML, Jett JR. Primary mediastinal tumors: part II. Tumors of the middle and posterior mediastinum. Chest. 1997; 112(5): p. 1344-57.
- Takeda S, Miyoshi S, Minami M, et al. Clinical spectrum of mediastinal cysts. Chest. 2003; 124(1): p. 125-32.
- Nessa KS. Imaging of Anterior Mediastinal Masses in Adults. J Cancer Sci and Therapy. 2017; 1(3).
- Chataigner O, Gossot D, Validire P, et al. [Mediastioscopic management of pleuropericardial cysts]. Rev Mal Respir. 2001; 18(1): p. 66-7.
- Temizkan V, Onan B, Inan K, et al. Hemorrhage into a pericardial cyst and associated right ventricular compression after blunt chest trauma. Ann Thorac Surg. 2010; 89(4): p. 1292-5 DOI: 10.1016/j.athoracsur.2009.09.018.
- GRIS D. The mediastinum. A text book of Radiology and Imaging. 6th, Vol. I ed. 1998, New York: Churchill Livingstone.
- Smahi M, Serraj M, Lakranbi M, et al. [Giant dumbbell shaped pleuropericardial cyst]. J Radiol. 2010; 91(12 Pt 1): p. 1295-6.
- Brown LR, Aughenbaugh GL. Masses of the anterior mediastinum: CT and MR imaging. AJR Am J Roentgenol. 1991; 157(6): p. 1171-80 DOI: 10.2214/ajr.157.6.1950860.
- Kuhlman JE, Fishman EK, Wang KP, et al. Mediastinal cysts: diagnosis by CT and needle aspiration. AJR Am J Roentgenol. 1988; 150(1): p. 75-8 DOI: 10.2214/ajr.150.1.75.
- Klatte EC, Yune HY. Diagnosis and treatment of pericardial cysts. Radiology. 1972; 104(3): p. 541-4 DOI: 10.1148/104.3.541.
- Pineda V, Andreu J, Cáceres J, et al. Lesions of the cardiophrenic space: findings at cross-sectional imaging. Radiographics. 2007; 27(1): p. 19-32 DOI: 10.1148/rg.271065089.
- Brunner DR, Whitley NO. A pericardial cyst with high CT numbers. AJR Am J Roentgenol. 1984; 142(2): p. 279-80 DOI: 10.2214/ajr.142.2.279.
- Elamin WF, Hannan K. Pericardial cyst: an unusual cause of pneumonia. Cases J. 2008; 1(1): p. 26 DOI: 10.1186/1757-1626-1-26.
- Jost RG. Computed tomography of the thorax. Radiology. 1978; 126(1): p. 125-36 DOI: 10.1148/126.1.125.
- Kaimal KP. Computed tomography in the diagnosis of pericardial cyst. Am Heart J. 1982; 103(4 Pt 1): p. 566-7.
- Peebles CR, Shambrook JS, Harden SP. Pericardial disease--anatomy and function. Br J Radiol. 2011; 84 Spec No 3: p. S324-37 DOI: 10.1259/bjr/16168253.
- Pugatch RD. CT diagnosis of pericardial cysts. AJR Am J Roentgenol. 1978; 131(3): p. 515-6 DOI: 10.2214/ajr.131.3.515.
- Verhaert D1, Gabriel RS, Johnston D, et al. The role of multimodality imaging in the management of pericardial disease. Circ Cardiovasc Imaging. 2010; 3(3): p. 333-43 DOI: 10.1161/CIRCIMAGING.109.921791.
- Wang ZJ, Reddy GP, Gotway MB, et al. CT and MR imaging of pericardial disease. Radiographics. 2003; 23 Spec No: p. S167-80 DOI: 10.1148/rg.23si035504.
- Fisher JK. Computed tomographic diagnosis of volvulus in intestinal malrotation. Radiology. 1981; 140(1): p. 145-6 DOI: 10.1148/radiology.140.1.7244217.
- Khurana B. The whirl sign. Radiology. 2003; 226(1): p. 69-70 DOI: 10.1148/radiol.2261011392.
- Hynes JK, Tajik AJ, Osborn MJ, et al. Two-dimensional echocardiographic diagnosis of pericardial cyst. Mayo Clin Proc. 1983; 58(1): p. 60-3.
- Padder FA, Conrad AR, Manzar KJ, et al., Echocardiographic diagnosis of pericardial cyst. Am J Med Sci. 1997; 313(3): p. 191-2.
- Portillo-Carroz K, Miguel-Campos E, Montoliú Tarramera R. [Pericardial cyst: all's well that ends well]. Rev Esp Cardiol. 2006; 59(10): p. 1082-3.
- Lewis KM, Sherer DM, Gonçalves LF, et al. Mid-trimester prenatal sonographic diagnosis of a pericardial cyst. Prenat Diagn. 1996; 16(6): p. 549-53 DOI: 10.1002/(SICI)1097-0223(199606)16:6<549::AID-PD879>3.0.CO;2-9.
- Le Bas JF, Rose-Pittet L, Brambilla E,et al. [MRI and tumors of the mediastinum. Correlation with CT x-ray]. J Radiol. 1987; 68(2): p. 81-8.
- Laurent F. Mediastinal masses: diagnostic approach. Eur Radiol. 1998; 8(7): p. 1148-59 DOI: 10.1007/s003300050525.
- Vinee P. MR imaging of the pericardial cyst. J Magn Reson Imaging. 1992; 2(5): p. 593-6.
- Abu Bakar N, Abdul Aziz YF, Singh Sandhu R, et al. Imaging of an atypical pericardial cyst. Heart Lung Circ. 2013; 22(4): p. 305-8 DOI: 10.1016/j.hlc.2012.07.016.
- Beroukhim RS, Prakash A, Buechel ER, et al. Characterization of cardiac tumors in children by cardiovascular magnetic resonance imaging: a multicenter experience. J Am Coll Cardiol. 2011; 58(10): p. 1044-54 DOI: 10.1016/j.jacc.2011.05.027.
- Nadkarni SCAJ. Case report - Mesothelial cyst of mediastinum. WJPLS. 2017; 3(10): p. 123-128.
- Parienty RA, Fontaine Y, Dufour G. Transformation of a pericardial cyst observed on long-term follow-up. J Comput Tomogr. 1984; 8(2): p. 125-8.
- Francese C, Schlumberger M, Travagli JP, et al., Iodine 131 uptake in a pleuropericardial cyst: case report of a false-positive radioiodine total body scan result in a patient with a thyroid cancer. Eur J Nucl Med. 1991; 18(9): p. 779-80.
- Jia C, Moadel R, Freeman LM. Focal thoracic uptake mimicking lung metastasis on 131I post-therapy whole-body scan in patients with thyroid carcinoma. Clin Nucl Med. 2014; 39(4): p. 360-2 DOI: 10.1097/RLU.0b013e31829959ce.
- Kinoshita Y, Shimada T, Murakami Y, et al. Ethanol sclerosis can be a safe and useful treatment for pericardial cyst. Clin Cardiol. 1996; 19(10): p. 833-5.
- Stoller JK, Shaw C, Matthay RA. Enlarging, atypically located pericardial cyst. Recent experience and literature review. Chest. 1986; 89(3): p. 402-6.
- Mouroux J, Padovani B, Maalouf J, et al. Pleuropericardial cysts: treatment by videothoracoscopy. Surg Laparosc Endosc. 1996; 6(5): p. 403-4.
- Esme H, Eren S, Sezer M, et al. Primary mediastinal cysts: clinical evaluation and surgical results of 32 cases. Tex Heart Inst J. 2011; 38(4): p. 371-4.
- Michelotto E, Tarantino N1, Ostuni V, et al. An Uncommon Pericardial Cyst in the Central Mediastinum: Incremental Diagnosis with Contrast-Enhanced Three-Dimensional Transesophageal Echocardiography. J Cardiovasc Echogr. 2013; 23(4): p. 106-110 DOI: 10.4103/2211-4122.127412.
- Salyer DC, Salyer WR, Eggleston JC. Benign developmental cysts of the mediastinum. Arch Pathol Lab Med. 1977; 101(3): p. 136-9.
- Ionescu LCD, Danila R, Radulescu C, et al Ectopic thymoma mimicking a pleuropericardial cyst: a case report. Eur Surg. 2010; 42(4): p. 194-196.
- Razemon PRM. Chirurgie du médiastin. Paris: Masson. 1970; p. 133-9.
- Demmy TL, Krasna MJ, Detterbeck FC, et al. Multicenter VATS experience with mediastinal tumors. Ann Thorac Surg. 1998; 66(1): p. 187-92.
- Hermens FH, Visser FJ, Termeer A, et al. Video assisted thoracoscopic treatment of pleuropericardial cysts. Diagn Ther Endosc. 2001; 7(2): p. 47-53 DOI: 10.1155/DTE.7.47.
- Kaul P, Javangula K, Farook SA. Massive benign pericardial cyst presenting with simultaneous superior vena cava and middle lobe syndromes. J Cardiothorac Surg. 2008; 3: p. 32 DOI: 10.1186/1749-8090-3-32.
- Landreneau RJ, Dowling RD, Castillo WM, et al. Thoracoscopic resection of an anterior mediastinal tumor. Ann Thorac Surg. 1992; 54(1): p. 142-4.
- Liu HP, Yim AP, Wan J, et al. Thoracoscopic removal of intrathoracic neurogenic tumors: a combined Chinese experience. Ann Surg. 2000; 232(2): p. 187-90.
- Roviaro G, Varoli F, Nucca O, et al. Videothoracoscopic approach to primary mediastinal pathology. Chest. 2000; 117(4): p. 1179-83.
- Bilal AIM, Khan MS. Experience of surgical management of mediastinal masses in a thoracic surgical unit of a tertiary care hospital. Pak J ChestMed. 2017; 23(3): p. 101-6.
- Szinicz G. Thoracoscopic resection of a pericardial cyst. Thorac Cardiovasc Surg. 1992; 40(4): p. 190-1 DOI: 10.1055/s-2007-1020146.
- Lang-Lazdunski L, Pilling J. Videothoracoscopic excision of mediastinal tumors and cysts using the harmonic scalpel. Thorac Cardiovasc Surg. 2008; 56(5): p. 278-82 DOI: 10.1055/s-2008-1038630.
- Hazelrigg SR. Thoracoscopic resection of mediastinal cysts. Ann Thorac Surg. 1993; 56(3): p. 659-60.
- Sugarbaker DJ. Thoracoscopy in the management of anterior mediastinal masses. Ann Thorac Surg. 1993; 56(3): p. 653-6.
- Yim AP. Video-assisted thoracoscopic resection of anterior mediastinal masses. Int Surg. 1996; 81(4): p. 350-3.
- Melfi F, Fanucchi O, Davini F, et al. Ten-year experience of mediastinal robotic surgery in a single referral centre. Eur J Cardiothorac Surg. 2012; 41(4): p. 847-51 DOI: 10.1093/ejcts/ezr112.
- Friday RO. Paracardiac cyst: diagnosis by ultrasound and puncture. JAMA. 1973; 226(1): p. 82.
- Unverferth DV, Wooley CF. The differential diagnosis of paracardiac lesions: pericardial cysts. Cathet Cardiovasc Diagn. 1979; 5(1): p. 31-40.
- Westcott JL. Percutaneous needle aspiration of hilar and mediastinal masses. Radiology. 1981; 141(2): p. 323-9 DOI: 10.1148/radiology.141.2.7291553.
- Menon P, Rao KL, Trehan A. Preoperative aspiration for anterior mediastinal cyst with respiratory distress. Indian Pediatr. 2003; 40(9): p. 897-900.
- Choi YW, McAdams HP, Jeon SC, et al. The "High-Riding" superior pericardial recess: CT findings. AJR Am J Roentgenol. 2000; 175(4): p. 1025-8.
- Pop D, Venissac N, Leo F, et al. Varicose pericardial vein: an unusual cause of right paracardiac opacity. J Thorac Cardiovasc Surg. 2005; 129(2): p. 448-9.
- Oldham HN Jr. Mediastinal tumors and cysts. Ann Thorac Surg. 1971; 11(3): p. 246-75.
- Nadkarni SCaJ. Case report - Mesothelial cyst of mediastinum. WJPLS. 2017; 3(10): p. 123-128.
- Hattori H. High prevalence of estrogen and progesterone receptor expression in mediastinal cysts situated in the posterior mediastinum. Chest. 2005; 128(5): p. 3388-90.
- Glazer HS, Siegel MJ, Sagel SS. Low-attenuation mediastinal masses on CT. AJR Am J Roentgenol. 1989; 152(6): p. 1173-7.
