Troponin Assay in the Real World: Is it Always a Diagnosis of Acute Myocardial Infarction?
Aidan (Jia Sheng) Yu1*, James Nguyen1, Anthony Brown2
1Royal Brisbane and Women’s Hospital Butterfield Street and Bowen Bridge Road, Herston, Queensland, 4029, Australia
2Gold Coast University Hospital, 1 Hospital Blvd, Southport QLD 4215
Abstract
Background: The soon to be implemented state-wide introduction of high-sensitivity troponin assays will allow the use of a lower threshold in identifying patients with acute myocardial infarction (AMI). Whether this assay will be too sensitive and therefore produce increased false positive results is still unclear. We aim to investigate whether a significantly elevated cardiac troponin using the current troponin assay (cTnI) will result in a clinical diagnosis of AMI.
Methods: A retrospective study was performed at a Queensland Hospital with all cTnI ordered across a single month reviewed. Patients who were diagnosed with Non ST-Elevation Myocardial Infarction or ST-Elevation Myocardial Infarction were labelled as having an AMI.
Results: In total, 944 investigations were ordered for 628 patients. Using the hospital laboratory cutoff of >0.040 μg/L(>99th percentile) for significance, a positive result was obtained in 105 patients (16.7%) and a negative result in 523 patients (83.3%). The positive troponin results were attributed to AMI (20%), congestive heart failure (20%), sepsis (19%), tachyarrhythmias (16.2%), renal failure (8.6%), airway disease (8.6%), pulmonary embolism (3.8%) and others - pericarditis, post angioplasty etc (3.8%). cTnI was found to be highly sensitive (100%, 95%CI 84-100%) and specific (86%, 95%CI 83-89%) for AMI. However, only 21 (3.3%) of 628 patients investigated received a diagnosis of AMI. The positive predictive value was poor (20%, 95% CI 13-29%), with the negative predictive value absolute (100%, 95% CI 99-100%).
Conclusion: Current troponin assays were found to be highly sensitive and specific in diagnosing AMI. However, its poor positive predictive value may be contributed by inappropriate requests.
Introduction
Chest pain is one of the most common presenting complaints in emergency departments, with the Australian Institute of Health and Welfare (AIHW) estimating around 157,000 acute myocardial infarction (AMI) related hospital admissions a year1. The term myocardial infarction refers to cell death of cardiac myocytes caused by ischemia and can clinically present as chest pain, diaphoresis, jaw and upper extremity discomfort. Due to the numerous ways in which a patient with AMI can present, cardiac biomarkers (troponin I and T) play a pivotal role in the diagnosis of AMI2. A key component of diagnosing AMI consists of having the value of troponin that exceeds the 99th percentile of a reference control group2.
The use of troponin I (cTnI) is fairly limited in the first few hours of AMI as levels of cTnI can take about 6 hours to increase3. The sensitivity of cTn assays increases from 10% to 45% within the first hour of the onset of pain to more than 90% at 8 or more hours3. Specificity reduces from 87% to 80% from 1 to 12 hours after symptom onset3.
An increase in cTnI indicates myocardial damage; however, this is not restricted to myocardial damage from coronary plaque rupture/occlusion which would yield a diagnosis of AMI4. Myocardial damage can be associated with secondary ischaemic injury as well as non-ischaemic myocardial injury4,5. Thus, an elevation of cTnI is also often seen in other conditions such as sepsis, tachyarrhythmias, chronic kidney disease, congestive cardiac failure, chronic obstructive pulmonary disease, pericarditis, pulmonary embolism, intracranial haemorrhage, and endurance exercise, amongst others4,5.
The introduction of highly sensitive cTn assays (hscTn-I) permits the ability to detect troponin at a lower threshold which can help identify AMI at an earlier rate6,7. However, increased sensitivity comes at the expense of decreased specificity, leading to a decreased positive predictive value of AMI6,7. This could result in a larger proportion of positive troponin levels, further adding to many clinicians’ diagnostic difficulties6,7.
With the state-wide adoption of hscTn-I on the horizon, this study aims to investigate whether an elevated troponin using the current troponin assay levels actually correlate to the diagnosis of AMI.
Methods
All troponins ordered in an Australian district hospital across 1 month were reviewed. Initial troponin assays ordered were to evaluate for AMI in patients who complained of chest pain. Subsequent troponin assays ordered for the same patient were to evaluate troponin trend (Table 1). Positive troponin was defined as using the laboratory cutoff >0.040 μg/L (>99th percentile) for significance. Each patient who had a troponin test ordered was then reviewed using hospital electronic medical records. Patients who were given the impression or diagnosis of Non ST-Elevation Myocardial Infarction (NSTEMI) or ST-Elevation Myocardial Infarction (STEMI) by a treating doctor were labelled as having an acute myocardial infarction.
Results
In total, 944 cTnI investigations were ordered. These consisted of 378 single and 250 serial (≥2 cTnI) investigations (Table 1). In total, 331 female and 297 male patients (N = 628) with a mean age of 60 years (range = 13-100) had tests requested.
Table 1: Number of cTnI ordered per patient
| Number of cTnI ordered per patient | Number of patients |
|---|---|
| 1 | 378 |
| 2 | 204 |
| 3 | 33 |
| ≥4 | 13 |
| Total 628 |
Using the hospital laboratory cutoff of >0.040 μg/L (>99th percentile) for significance, a positive result was obtained in 105 patients (16.7%) and a negative result in 523 patients (83.3%). The positive troponin results were attributed to AMI (20%), congestive heart failure (20%), sepsis (19%), tachyarrhythmias (16.2%), renal failure (8.6%), airway disease (8.6%), pulmonary embolism (3.8%) and others - pericarditis, post angioplasty, hypoglycaemia, polypharmacy etc (3.8%) (Figure 1).
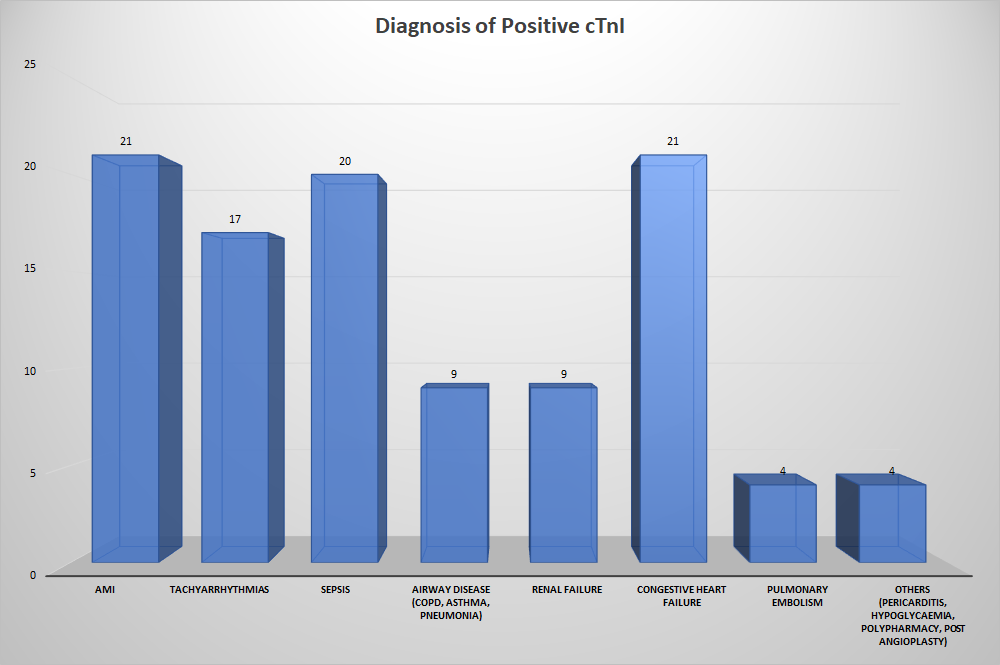
Figure 1: Diagnosis given to patients with positive cTnI
cTnI was found to be both highly sensitive (100%, 95% CI 84-100%) and specific (86%, 95% CI 83-89%) for AMI. However, only 21 of 628 patients received a diagnosis of AMI, yielding a diagnostic rate of 3.3%. The positive predictive value was poor (20%, 95% CI 13-29%), with the negative predictive value absolute (100%, CI 99-100%).
Discussion
The use of troponin testing plays an important role in the diagnosis and evaluation of AMI with a positive value exceeding the 99th percentile of a reference control group. The 1% threshold for the positive value of a troponin level, should always be used in the clinical context and is more valuable in individuals with a high pre-test probability2. Positive troponin assays are an indicator of myocardial inflammation or transient myocardial ischaemia and therefore multiple causes, other than AMI, can also be attributed to the result4,5.
The following list, although not exhaustive, lists possible causes of an elevated troponin.
Sepsis
A positive troponin can be found in approximately 61% of septic patients8 and 43% of patients in an intensive care unit9. A mismatch in supply and demand, secondary to hypotension, tachycardia and hypoxemia, leads to decreased myocardial perfusion and subsequent release of troponin. Myocarditis may also occur in sepsis due to cytokine and endotoxin release resulting in increased cell membrane permeability and myocardial depression10.
Pulmonary Embolus
Patients with pulmonary embolism (PE) can present with similar symptoms of AMI such as chest pain and shortness of breath. This is further complicated by the fact that approximately 50% of patients with a PE have an elevated troponin11. The rise in troponin is attributed to decreased perfusion of the coronary arteries, overflow of the right ventricle and hypoxemia. Although troponin testing is generally reserved for diagnostic purposes, it has been shown that an elevated troponin in patients with PE plays an important prognostic role as this can predict right ventricular heart strain and an increased number of segmental perfusion defects on lung scintigraphy12. A prospective study of 56 patients with PE revealed that a cTnT tested within 12 hours of presentation was elevated in 32% of patients with a moderate or massive PE. The prevalence of cardiogenic shock, need for resuscitation, ionotropic support and mechanical ventilation were all higher in the group with a raised troponin13.
Pulmonary Embolus
Cardiac complications are the most common cause of death in end stage renal failure patients and an elevated troponin can be seen in largely asymptomatic patients. In this subset of patients, cTnT is more regularly elevated than cTnI. Possible explanations of troponin elevation in dialysis patients include left ventricular hypertrophy14 or microinfarctions15. A large study showed that a raised troponin in dialysis patients coincided with a greater prevalence of severe coronary artery disease16 It has also been shown that an elevated troponin in dialysis patients prognostically increases the risk of death17,18.
Heart failure
Elevated troponins in patients with heart failure is a common finding and the mechanism behind it is multifactorial. Coronary artery disease is a common cause of heart failure, however serum troponins have also found to be raised in patients with no obstructive disease. This is likely due to subendocardial ischemia and inflammatory changes leading to myocyte damage. This is further exacerbated by tachycardia, hypotension, anaemia and arrhythmias19,20. As with other conditions such as PE and renal failure, an elevated troponin in acute heart failure has its own prognostic value. The Acute Decompensated Heart Failure National Registry (ADHERE) study analysed 67,924 patients from 274 hospitals. 4,240 (6.2%) of those patients had an elevated troponin on admission21. These patients were also found to have a lower blood pressure with a reduced left ventricular ejection fraction on presentation. An elevated troponin has also been associated with an increased risk of complications and mortality22.
Pericarditis
Elevated troponin levels can be found in up to 32% of patients with pericarditis23. An elevated troponin was associated with increased rates ST segment elevation and pericardial effusion. However, in a study of 118 patients with pericarditis, no negative prognostic value was shown23.
Cerebral vascular disease (CVA)
A systemic review of 15 studies revealed that 18.1% of acute stroke patients had an elevated troponin24. Possible mechanisms of troponin elevation in patients with CVA include increased catecholamine release secondary to increased sympathetic tone25 and a higher prevalence of atrial fibrillation, heart failure and renal disease. Multiple studies have shown a positive troponin level leads to adverse outcomes26,27.
Apical ballooning syndrome
Apical ballooning syndrome (ABS), also referred to as Takotsubo cardiomyopathy, poses a diagnostic dilemma for clinicians as the clinical presentation, ECG findings and biomarker levels can all mimic an AMI. The condition is due to an increase in catecholamine release triggered by an emotional or physical stressor. This subsequently causes transient contractile dysfunction and microvascular spasms. Studies have suggested that in patients with suspected ACS, 1-2% are eventually diagnosed with ABS28,29.
In this study, cTnI was found to be both highly sensitive (100%) and specific (86%) for AMI. However, only 3.3% of patients investigated received a diagnosis of AMI, which yielded a poor positive predictive value of 20%. Congestive heart failure was the second most common cause of cTnI elevation, followed by sepsis, tachyarrhythmias, renal failure, airway disease, and pulmonary embolism. Despite cTnI being highly sensitive and specific, the poor positive predictive value of the test likely stemmed from the possibility of inappropriate requests and lack of understanding of the myriad of causes for troponin elevation. For example, we found that 20% of patients who had a positive troponin were due to congestive heart failure. In patients with heart failure, continuous troponin release is a well-known phenomenon19,20. The likelihood of a positive troponin in these patients is high and troponin should only be ordered in patients who report typical chest pain suggestive of AMI. Inappropriate testing would not only result in significant financial burden to the hospital, but also result in unnecessary interventions and a delay in ascertaining the correct diagnosis. Similar findings were also found in other hospitals. An audit in three metropolitan Victorian Hospitals found that serial troponin testing was ordered appropriately as per the hospital protocol30. However, single troponin assay was ordered frequently and inappropriately. The authors found that 93% of the 194 single troponin assays ordered were not followed up with a second troponin, possibly due to initial overestimation of the diagnosis of AMI30. This suggested the possibility of clinicians utilising a single troponin assay as an exclusion criterion when faced with a diagnostic dilemma. An audit conducted in Royal Gwent Hospital in the UK also found troponin being used as a differentiating tool prior to clinical assessment in the emergency triage, resulting in numerous positive results in non-AMI patients31. In fact, only 6.1% of 213 troponin requests yielded a diagnosis of ACS31. This added unnecessary financial strain to the healthcare system.
These issues may further amplify with the introduction of hscTn-I which will provide a higher sensitivity at the expense of decreased specificity. One study found the use of hscTn-I resulted in significant rapid diagnosis of AMI, therefore reducing the time spent in the emergency department but without any change in admission rates6. However, it also resulted in an 8.2% increase in coronary angiography rate, although without an increased rate of coronary revascularisation or coronary artery bypass graft6. Nonetheless, there was no change in inhospital mortality6. A study which reclassified patients using hscTn-I whose troponin was below the diagnostic cut-off using contemporary assay found that an additional 17% of 10360 patients would have been classified as having positive troponin results. However, the additional diagnoses did not affect the incidence of cardiovascular death at 1 year7.
The findings of this study further expand upon previous literature, emphasising the fact that an adequate risk stratification of patients is fundamental for interpreting a positive troponin result. The low positive predictive value of cTnI found in this study likely stemmed from inappropriate request of the test. The test should only be ordered to ‘rule in’ a diagnosis of AMI after a comprehensive clinical assessment, rather than using it to ‘rule out’ the diagnosis of AMI. Dr. Robert Jesse, a cardiologist commented: “When troponin was a lousy assay it was a great test, but now that it's becoming a great assay, it's getting to be a lousy test.32” As troponin assays continue to improve its sensitivity, this will come at the cost of decreased specificity. Clinicians have to remember that it is a tool that will only be useful if the operator is able to interpret it in the appropriate clinical context. It is imperative that clinicians have an awareness of both ischaemic and non-ischaemic causes of troponin elevation.
Some limitations were identified in this study. This was a retrospective study that looked at the number of troponin assays ordered, meaning only patients with troponin ordered were evaluated. Although unlikely, patients with AMI but without a troponin ordered would have been omitted. This study relied on diagnoses that were given by clinicians and accurate documentation on the electronic medical records. Clinical outcomes other than diagnosis were not collected. Information such as ECG, echocardiography, CT coronary angiography, stress echocardiography and myocardial perfusion scan were not collected which would have allowed better assessment of underlying coronary artery disease. While a troponin increase is not synonymous of AMI, nevertheless coronary artery disease may not be excluded. With exclusion of conditions such as pulmonary embolism and congestive heart failure whom other pathophysiological mechanisms are involved, haemodynamic changes induced by the patient’s clinical condition may unmask “silent” severe coronary artery disease. Further information with these non-invasive cardiac imaging modalities could provide further information of underlying coronary artery disease. Moreover, description of population such as atherosclerotic risk factors and gender were not included and as such, subgroup analysis and comparison were omitted. In addition, only contemporary cTnI assay was evaluated in this study. The findings of our study represented the findings from one district hospital over a period of one month. The sensitivity of troponin for the diagnosis of AMI was 100% in this study due to a small population size and the two patients who had acute STEMI both had a positive first troponin assay. However, it is likely that if the population size was bigger, as acute STEMI should preferably be diagnosed before the elevation of troponin levels, the sensitivity of positive troponin levels will be less than 100%. A prospective study may have been performed more easily during this short period of time which would have allowed better collection of aforementioned data. However, this was made difficult due to state-wide change over of troponin assay to hscTn-I.
Conclusion
An elevated troponin in this study correlated well to the diagnosis of AMI. However, its poor positive predictive value was the result of multiple positive troponin assays found in patients with diagnoses other than AMI. This was likely due to inadequate clinical stratification strategy when ordering troponin and signified the ongoing need of better clinical assessment.
| LEGEND | |
|---|---|
| ABS | Apical Ballooning Syndrome |
| ACS | Acute Coronary Syndrome |
| AIHW | Australian Institute of Health and Welfare |
| AMI | Acute Myocardial Infarct |
| CI | Confidence Interval |
| CTNI | Cardiac Troponin I |
| CTNT | Cardiac Troponin T |
| CVA | Cerebrovascular Accident |
| ECG | Electrocardiography |
| HSCTN-I | High Sensitivity Cardiac Troponin I |
| NSTEMI | Non ST-Elevation Myocardial Infarction |
| PE | Pulmonary Embolism |
| STEMI | ST-Elevation Myocardial Infarction |
References
- AIHW. 3.6 Coronary heart disease. https://www.aihw.gov.au/getmedia/7ec2ec71-4af4-43cf-bdaf-e4b15a04f11d/aihw-aus-221-chapter-3-6.pdf.aspx
- Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J. 2019 Jan 14; 40(3): 237-269. doi: 10.1093/eurheartj/ehy462.
- Ebell MH, Flewelling D, Flynn CA. A systematic review of troponin T and I for diagnosing acute myocardial infarction. J Fam Pract. 2000 Jun; 49(6): 550-6.
- Rahman A, Broadley S. Review article: Elevated troponin: Diagnostic gold or fool's gold? Emergency Medicine Australia. 2014; 26(2): 125-30.
- Tanidi A, Cemri M. Troponin elevation in conditions other than acute coronary syndromes. Vascular Health and Risk Management. 2011; 7: 597-603.
- Yip TP, Pascoe HM, Lane SE. Impact of high-sensitivity cardiac troponin I assays on patients presenting to an emergency department with suspected acute coronary syndrome. Med J Aust. 2014 Aug 4; 201(3): 158-61.
- Shah ASV, Anand A, Strachan FE, et al. High-sensitivity troponin in the evaluation of patients with suspected acute coronary syndrome: a stepped-wedge, cluster-randomised controlled trial. Lancet. 2018 Sep 15; 392(10151): 919-928. doi: 10.1016/S0140-6736(18)31923-8.
- Bessière F, Khenifer S, Dubourg J, et al. Prognostic value of troponins in sepsis: a meta analysis. Intensive Care Med. 2013; 39: 1181–1189.
- Lim W, Qushmaq I, Devereaux PJ, et al. Elevated cardiac troponin measurements in critically ill patients. Arch Intern Med. 2006; 166: 2446–2454.
- Hussain N. Elevated cardiac troponins in setting of systemic inflammatory response syndrome, sepsis, and septic shock. ISRN Cardiol. 2013; 2013: 1–7.
- Kilinc G, Dogan OT, Berk S, et al. J Thorac Dis. 2012 Dec; 4(6): 588–593. doi: 10.3978/j.issn.2072-1439.2012.10.13.
- Meyer T, Binder L, Hruska N, et al. Cardiac troponin I elevation in acute pulmonary embolism is associated with right ventricular dysfunction. J Am Coll Cardiol 2000; 36: 632–6.
- Giannitsis E, Muller-Bardorff M, Kurowski V, et al. Independent prognostic value of cardiac troponin T in patients with confirmed pulmonary embolism. Circulation 2000; 102: 211–17.
- Mallamaci F, Zoccali C, Parlongo S, et al. Troponin is related to left ventricular mass and predicts all-cause and cardiovascular mortality in hemodialysis patients. Am J Kidney Dis. 2002; 40: 68–75.
- Antman EM. Decision making with cardiac troponin tests. N Engl J Med. 2002; 346: 2079–2082.
- deFilippi C, Wasserman S, Rosanio S, et al. Cardiac troponin T and C-reactive protein for predicting prognosis, coronary atherosclerosis, and cardiomyopathy in patients undergoing long-term hemodialysis. JAMA. 2003; 290: 353–359.
- Khan NA, Hemmelgarn BR, Tonelli M, et al. Prognostic value of troponin T and I among asymptomatic patients with end- stage renal disease: a meta-analysis. Circulation. 2005; 112: 3088–3096.
- Apple FS. Predictive value of cardiac troponin I and T for subsequent death in end-stage renal disease. Circulation. 2002; 106: 2941–2945.
- Kociol RD, Pang PS, Gheorghiade M, et al. Troponin elevation in heart failure prevalence, mechanisms, and clinical implications. J Am Coll Cardiol. 2010; 56: 1071–8.
- Januzzi JL Jr, Filippatos G, Nieminen M, et al. Troponin elevation in patients with heart failure: on behalf of the third Universal Definition of Myocardial Infarction Global Task Force: Heart Failure Section. Eur Heart J. 2012; 33: 2265–71.
- Peacock WF, De Marco T, Fonarow GC, et al. Cardiac troponin and outcome in acute heart failure. N Engl J Med. 2008; 358: 2117–26.
- You JJ, Austin PC, Alter DA, et al. Relation between cardiac troponin I and mortality in acute decompensated heart failure. Am Heart J. 2007; 153: 462–70.
- Imazio M, Demichelis B, Cecchi E, et al. Cardiac troponin I in acute pericarditis. J Am Coll Cardiol. 2003; 42(12): 2144-2148.
- Kerr G, Ray G, Wu O, et al. Elevated troponin after stroke: a systematic review. Cerebrovasc Dis. 2009; 28(3): 220-6. doi: 10.1159/000226773.
- Samuels MA. The brain-heart connection. Circulation. 2007; 116: 77–84. doi: 10.1161/CIRCULATIONAHA.106.678995.
- Di Angelantonio E, Fiorelli M, Toni D, et al. Prognostic significance of admission levels of troponin I in patients with acute ischaemic stroke. J Neurol Neurosurg Psychiatry. 2005; 76: 76–81.
- Ghali J, Allison D, Kleinig T, et al. Elevated serum concentrations of troponin T in acute stroke: what do they mean. J Clin Neurosci. 2010; 17: 69–73.
- Kurowski V, Kaiser A, von Hof K, et al. Apical and midventricular transient left ventricular dysfunction syndrome (tako-tsubo cardiomyopathy): frequency, mechanisms, and prognosis. Chest. 2007; 132: 809–16.
- Gianni M, Dentali F, Grandi AM, et al. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J. 2006; 27: 1523–9.
- Davey RX. Troponin testing: an audit in three metropolitan hospitals. Med J Aust. 2003 Jul 21; 179(2): 81-3.
- Gardezi SA. Troponin: think before you request one. BMJ Qual Improv Rep. 2015 Mar 25; 4(1). pii: u204560.w3221. doi: 10.1136/bmjquality.u204560.w3221.
- Jesse RL. On the relative value of an assay versus that of a test: a history of troponin for the diagnosis of myocardial infarction. J Am Coll Cardiol. 2010 May 11; 55(19): 2125-8. doi: 10.1016/j.jacc.2010.03.014.
