Acute Myocardial Readmission Reduction Program: “Never Discharge A Patient”
Deepti Bhandare1*, Thomas Shimshak2
1Department of Cardiology, Advent Health Sebring, Sebring, Florida
2Department of Interventional Cardiology, Advent Health Sebring, Florida
Abstract
Readmission for Acute Myocardial Infarction [AMI] significantly contributes to preventable morbidity and healthcare costs. Nearly 1 in 6 patients hospitalized with AMI have an unplanned readmission within 30 days of discharge, accounting for over $1 billion of annual US healthcare costs. We developed a unique integrated product in our hospital called “Transition of Care” program [TOC] with the help of technology and services from Patient Engagement Advisors. The TOC program was based on the notion that engaging patients in their self-care journey by provision of extended set of products and facilities, nutrition, medications, and services to meet their care and recovery needs across the continuum of care.
The TOC program led to the subsequent reduction in the AMI readmission and significant cost savings by avoiding Medicare penalties. AMI readmission rates were reduced to less than 20% since implementation and have fallen below expected rates. This has translated to more than $ 400,000 savings in penalties as the actual readmission rate has been under the expected rate.
It also led to improved clinical follow up in the post AMI patients and improvement in clinical parameters in patients with chronic conditions like diabetes and hypertension. The TOC program extends health care beyond the four walls of the medical care facility and never truly discharges the patient.
Abbreviations
AMI: Acute Myocardial Infarction; ACS: Acute coronary syndrome; TOC: Transition of Care; PEA: Patient Engagement Advisors; AHS: Advent Health Sebring; TS: Transition specialist; PNS: Patient Navigation System; SNF: Skilled nursing facility; ALF: Assisted Living facility; UDMI: Universal Definition of Myocardial Infraction
Background
The Hospital Readmissions Reduction Program (HRRP) is a Medicare value-based purchasing program that decreases monetary expenditures to hospitals with excess readmissions1. The program supports the national goal of refining healthcare for Americans by relating payment to the quality of hospital care2. Hospitals are subjected to federal financial penalties for excessive 30-day hospital readmissions for acute myocardial infarction (AMI). Readmission after hospitalization for AMI significantly contributes to preventable morbidity and health-care costs3. Quality of care utilization measures for patients admitted to the hospital with an AMI includes the length of stay and 30-day readmission rates.
Advent Health Sebring [AHS], a community-based hospital developed a robust Transitions of Care (TOC) program requiring technology and service assistance from Patient Engagement Advisors (PEA).
Founded in 2008, PEA partners with forward thinking healthcare organizations to successfully provide healthcare solutions which are individualized to each patient's healthcare needs. Engaging patients in their self-care journey by providing an expanded set of products, nutrition, medications, and services to meet their care and recovery needs across the continuum of care.
This includes preventative health management support, clinical guidance and enrollment into activities that support a successful acute experience, interventional and discharge coordination including discharge medications, necessary alignment with self-care products, nutrition, and follow-up service appointments (i.e. home care, rehabilitation, primary care, medication or nutrition therapy management).
Aim
Our aim was to test whether using the TOC program resulted in reduced 30-day readmission after AMI in a community-based hospital. The secondary aims were to evaluate for improvement in post hospital discharge follow ups in the outpatient clinics.
Methods
PEA developed with AHS an implementation and governance plan called TOC program that incorporates senior leadership support, technology and several key operational processes including pharmacy, home care and physician service, nursing, case management, outpatient services, marketing, finance and legal.
A team of pharmacy technicians was hired called ‘Transition Specialists’ [TS] to staff all clinical settings across the campus, providing in-person and telephonic support 24x7, 7 days a week. TS carry an iPad with proprietary built an application called Patient Navigation System (PNS) interfaced with admissions/discharge teams, diagnosis, retail pharmacy and ambulatory systems.
The team first developed a branded enrollment program named TOC. A highly developed process of engaging all patients and enrolling them into the formality of a program with the intent to reduce out of pocket expenses for required items such as medications, enhance convenience, improve safety and quality of care. The expression of interest to maintain the relationship with the patient into perpetuity and well beyond discharge is a key component.
The targeted patients are rolled out in phases:
* Phase 1: ER, Observation and Acute discharges
* Phase 2: Skilled Nursing Facility (SNF) and Assisted Living Facility (ALF) discharges to home
* Phase 3: Home Health / In Home Integration
The PNS systems load all high-risk populations (inclusive of AMI) and allow the team to prioritize their day accordingly. Each TS participates in multi-disciplinary rounds with physicians, case management, nursing and allied service teams to gather needed subjective information while assessing discrete objective information in the medical records. In addition, the TS assesses a full list of social determinant questions with each patient that then formulates a comprehensive action list.
Services provided: Treating the “Whole patient”.
The team has primary fulfillment and delivery logistics tied to developed action lists, which include:
1. Scheduled follow up appointments with primary care and/or specialists. This also included the expectation setting for post-acute services [Home Health/SNF/ALF processes aligned with TOC.
2. Coordination of transportation logistics from home to clinics.
3. Medications (discharge medications brought to bedside, mail order, working on prior authorizations, eligibility for free medications, obtaining patient assistance from drug companies, saving significant out of pocket expense for patients)
4. Nutrition support (providing in home clinically built meals in 7,14,21-day increments-low sodium diets, diabetic diet).
5. Clinical products/kits (customized kits built to preferences including blood pressures cuffs scales, oximeter, medication organizers etc).
6. Analytics/performance team
A combination of alerting mechanisms through the PNS system allows real time notifications for missed patients and follow up requirements needed to support high risk AMI patients. Daily evaluations of analytic tools and generate reports from a team of analysts are submitted to aid operational teams as they evaluate support, eligibility, contract requirements, productivity and effectiveness. Readmission comparatives are embedded into daily operation calls across all departments and clinical, finance and executive meetings.
This was a small sized retrospective study. Patients with AMI who underwent percutaneous intervention were eligible for the study from a period of November 2017 to October 2018. Patients with AMI who had not received any interventional therapy were excluded from the study. The AMI patients registered in the TOC program received assistance with coordination of physicians [primary care physicians and specialists] appointments, transportation logistics, medications assistance, nutrition support and home clinical kits [Figure 1].
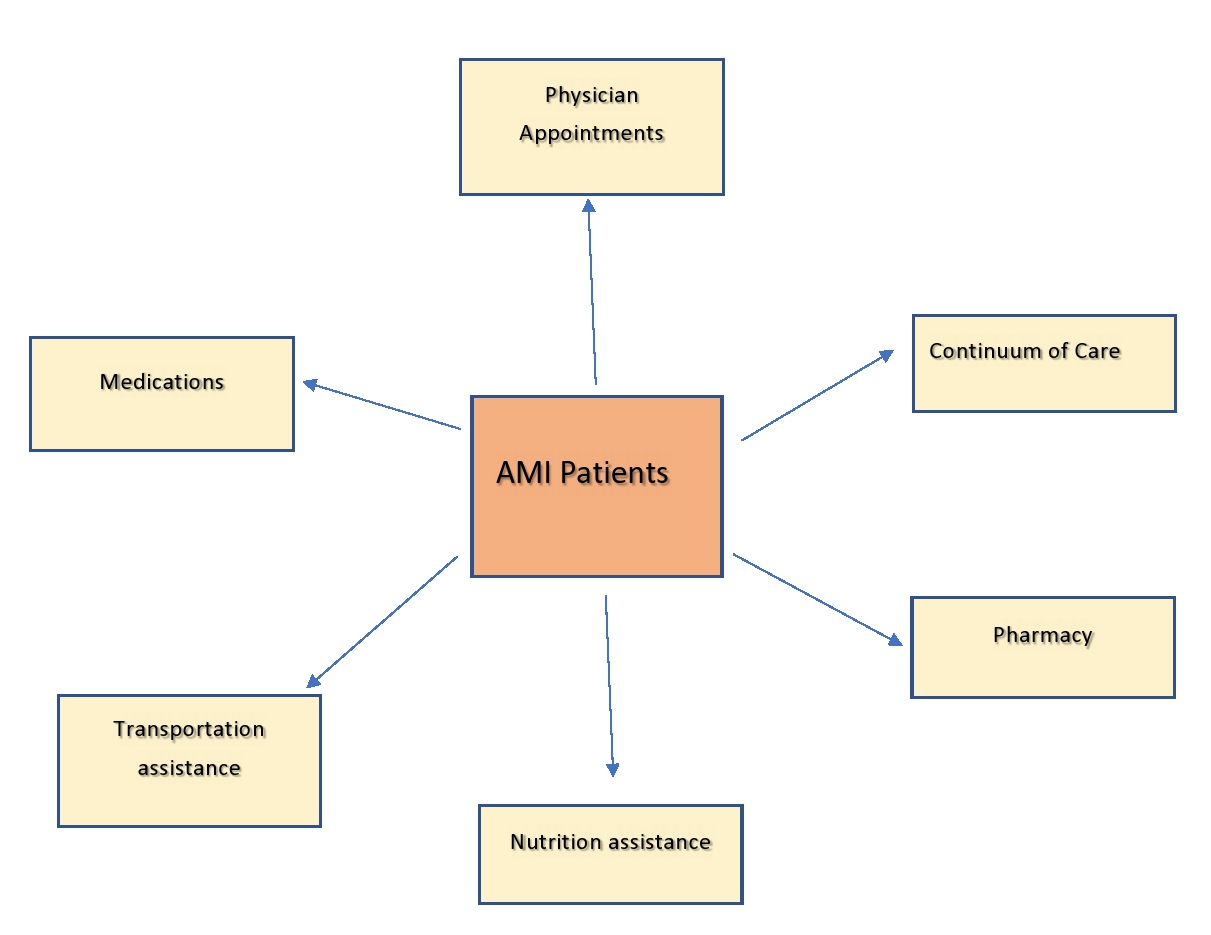
Figure 1:
Hospital readmissions were measured for AMI patients readmitted to Advent Health Sebring for all cause and not just cardiac specific cause. The readmission data was obtained from the medical charts on electronic health records review by the Quality department.
Results
The TOC program was started in November 2017. This was a pilot project started in our hospital. 95% of all the AMI patients who fit the inclusion criteria were offered the TOC program. 99% of the AMI patients voluntarily accepted and enrolled in the TOC program which were 880 in number. Nearly half of the patients were in the 75 years and older age group. The readmissions were also the highest in the 75 and older age group [Table 1]. AMI readmission rates have reduced to less than 20% since implementation and fallen below expected rates for the fiscal year November 2017 to October 2018, which translates to more than $ 400,000 savings in penalties. The readmission rate prior to the TOC program was 42% for the previous annual year. The observed 30-day readmission rate has been under the expected rate. [Figure 2].
Table 1:
|
Standard age grouping |
Total cases enrolled: 880 |
Age specific Readmissions: 174 |
|
18 through 64 years |
219 (24.9 %) |
53 (30.5 %) |
|
65 through 74 years |
241 (27.4 %) |
45 (25.8 %) |
|
75 years and older |
420 (47.7 %) |
76 (43.7 %) |
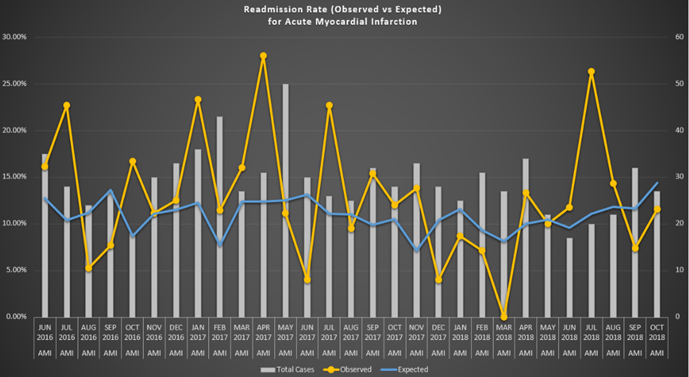
Figure 2:
The excess readmission ratio for AMI was <1 (0.8882). Scheduled appointments prior to discharge have increased from 27% to 80%. 90% of all patients are showing up for scheduled appointments. The no show rate prior to TOC program was 35-40%.
Due to an increase in the outpatient appointments for new and follow up patients, there has been an increase in financial returns for the hospital. The TOC program helped improve the quality of care for other chronic illnesses like diabetes and hypertension.
Since the success of the PEA pilot project, the TOC project has been successfully extended into the other hospitals in the Advent Health System.
Discussion
The Hospital Readmission Reduction Program was enacted under Section 3025 of the Patient Protection and Affordable Care Act in March 2010 and imposed financial penalties beginning in October 2012 for hospitals with higher-than-expected readmissions for AMI, congestive heart failure and pneumonia among their fee-for-service Medicare beneficiaries. Since the program’s inception, thousands of hospitals have been subjected to penalties now totaling nearly $1 billion1-3.
Acute coronary syndromes include unstable angina pectoris and AMI. The electrocardiogram (ECG) is used to triage patients with ACS into ST segment elevation myocardial infarction and non-ST segment myocardial infarction. ACS develops due to atherosclerotic obstruction in the coronary arteries. AMI can occur in varied clinical situations occur under similar clinical circumstances. Acknowledgement of the clinical intricacy of ACS has directed main administrations of cardiologists to join hands and develop criteria for the diagnosis and treatment of AMI. In 2000, the Universal Definition of Myocardial Infraction [UDMI] was founded on the redefinition of AMI as myocardial injury observed by elevated serum cardiac biomarkers [cardiac troponin] in acute myocardial ischemia. In 2007, the second UDMI demonstrated a novel AMI classification with five categories followed by a third UDMI with amendments related to coronary interventions. In 2018, the fourth update of UDMI was published in relationship to the introduction and widespread use of high sensitivity cardiac troponin assays4.
The UDMI classifies AMI according to a combination of pathophysiology and clinical setting as follows: AMI occurring in relationship to a primary atherothrombotic coronary event (type 1), supply and demand mismatch (type 2), sudden cardiac death (SCD) (type 3), percutaneous coronary intervention (PCI) (type 4A), coronary stent thrombosis (type 4B), and coronary artery bypass graft surgery (type 5)5.
In the newest statement, major importance has been given to the levels of high sensitivity cardiac troponin. Utilization of the high sensitivity cardiac troponin assays has changed the scientific approach to the valuation of AMI and differential diagnosis even though the clinical criteria for AMI have not been altered6.
In our study, any patient with ACS who underwent percutaneous coronary intervention was eligible to participate in the TOC program. We did not use high sensitivity cardiac troponin assays in our hospital. The 30-day readmission could be due to any cause not limited to cardiac specific cause.
To reduce costs and improve healthcare quality, the United States government has put increasing pressure on hospitals to decrease preventable readmissions7. Starting in 2009, Medicare publicly reported hospital 30-day risk-standardized readmission rates for heart failure, AMI, and pneumonia on its Hospital Compare website8. In 2012, following the passage of the Affordable Care Act, the federal government began directing financial penalties toward hospitals with higher-than-expected 30-day readmission rates for these three conditions. These penalties have increased each year since 2012; this year, total Medicare payments may be reduced up to 3% for hospitals with the highest 30-day readmission rates for publicly reported conditions9.
Despite these changes, the scientific literature has not provided clear guidance on the best ways to reduce preventable rehospitalizations10. Studies identifying risk factors have found inconsistent results; published predictive models have had only poor to fair discriminative capacity; and intervention studies have generally been limited by their small sample size and local context-dependent factors. Findings have been heterogeneous and are difficult to generalize11,12.
Hospital readmissions for AMI depend more on compound relations between patient, hospital, community, and environment rather than on clinical severity of illness alone13. In certain conditions such as heart failure and pneumonia, including more data on socioeconomic and psychosocial factors improved prediction of 30-day readmission risk14,15.
The focus of the TOC program was since patients need to play an increased role in their health and health care decision-making in order to achieve the optimal benefits. The argument that we as healthcare providers, could provide "perfect care" could be derailed by the patient not holding up their end of the bargain (like adhering to medications).
TOC uniquely understand the complexities that support and reinforce the provider/patient relationship by focusing first on patient treatment and self-care needs, second on service, medication, nutrition, and product alignment, and third on the collection, reimbursement, and margin optimization.
The expression of interest to maintain the relationship with the patient into perpetuity well beyond discharge is a key component.
Our study was a small retrospective study done as a pilot project. Under the TOC program the observed 30-day readmission rate has been under the expected rate and the excess readmission ratio for AMI was <1 (0.8882) which is comparable to study done by Marbach JA et al13.It is a limited study due to small size and inability to obtain data on the socioeconomic and financial status.
Conclusions
Readmissions for patients with AMI were reduced since the implementation of TOC program. The observed 30-day readmission rate has been under the expected rate. The excess readmission ratio for AMI was <1 (0.8882). This has contributed to significant savings for the hospital by preventing the penalty payments under the Hospital Readmission Reduction Program. The TOC program extends commitment to care for patients and caregivers beyond the hospital walls and truly never discharges a patient.
Disclosures
Dr Shimshak: Boston Scientific, Endologix.
References
- https://www.cms.gov/Medicare/Medicare-Fee-for-Service Payment/AcuteInpatientPPS/Readmissions-Reduction-Program
- Lauren N Smith, Anil N Makam, Douglas Darden, et al. Acute Myocardial Infarction Readmission Risk Prediction Models A Systematic Review of Model Performance. Circulation: Cardiovascular Quality and Outcomes. January 2018; Volume 11, Issue 1.
- Elizabeth H Bradley, Harlan M Krumholz. Contemporary Evidence About Hospital Strategies for Reducing 30-Day readmissions. A National Study. J Am Coll Cardiol. August 2012; Volume 60, Issue 7.
- Buja LM, Zehr B, Lelenwa L, et al. Clinicopathological complexity in the application of the universal definition of myocardial infarction. Cardiovasc Pathol.2020; 44: 107153. doi:10.1016
- Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018).Circulation. 2018; 138: e618-e651.
- Twerenbold R, Boeddinghaus J, Nestelberger T, et al. Clinical Use of High-Sensitivity Cardiac Troponin in Patients With Suspected Myocardial Infarction. J Am Coll Cardiol. 2017; 70(8): 996–1012. doi:10.1016
- Kumar Dharmarajan, Harlan Krumholz. Strategies to Reduce 30-Day Readmissions in Older Patients Hospitalized with Heart Failure and Acute Myocardial Infarction. Curr Geriatr Rep. 2014 Dec 1; 3(4): 306–315.
- Ko DT, Khera R, Lau G, et al. Readmission and Mortality After Hospitalization for Myocardial Infarction and Heart Failure. J Am Coll Cardiol. 2020 Feb 25; 75(7): 736-746. doi: 10.1016
- Wasfy JH, Bhambhani V, Healy EW, et al. Relative Effects of the Hospital Readmissions Reduction Program on Hospitals That Serve Poorer Patients. Med Care. 2019 Dec; 57(12): 968-976. doi: 10.1097.
- Popescu I, Sood N, Joshi S, et al. Trends in the Use of Skilled Nursing Facility and Home Health Care Under the Hospital Readmissions Reduction Program: An Interrupted Time-series Analysis. Med Care. 2019 Oct; 57(10): 757-765. doi: 10.1097
- Panagiotou OA, Kumar A, Gutman R, et al. Hospital Readmission Rates in Medicare Advantage and Traditional Medicare: A Retrospective Population-Based Analysis. Ann Intern Med. 2019 Jul 16; 171(2): 99-106. doi: 10.7326/M18-1795.
- Wadhera RK, Joynt Maddox KE, Wasfy JH, et al. Association of the Hospital Readmissions Reduction Program With Mortality Among Medicare Beneficiaries Hospitalized for Heart Failure Acute Myocardial Infarction and Pneumonia. JAMA. 2018 Dec 25; 320(24): 2542-2552. doi: 10.1001
- Marbach JA , Johnson D, Kloo J, et al. The Impact of a Transition of Care Program on Acute Myocardial Infarction Readmission Rates. Am J Med Qual. 2018 Sep/Oct; 33(5): 481-486. doi: 10.1177
- Ryan AM, Krinsky S, Adler-Milstein J, et al. Association Between Hospitals' Engagement in Value-Based Reforms and Readmission Reduction in the Hospital Readmission Reduction Program. JAMA Intern Med. 2017 Jun 1; 177(6): 862-868. doi: 10.1001
- Desai NR, Ross JS, Kwon JY, et al. Association Between Hospital Penalty Status Under the Hospital Readmission Reduction Program and Readmission Rates for Target and Nontarget Conditions. JAMA. 2016 Dec 27; 316(24): 2647-2656. doi: 10.1001
